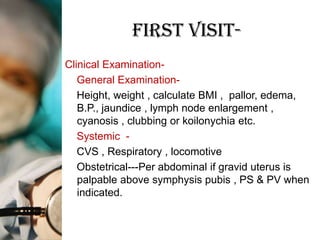
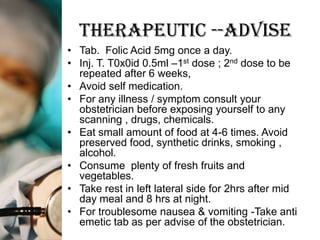
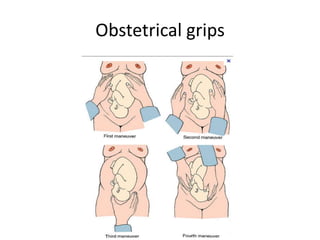
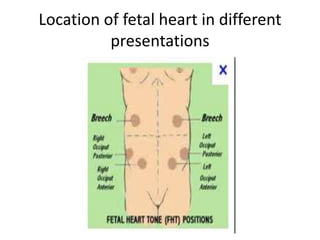
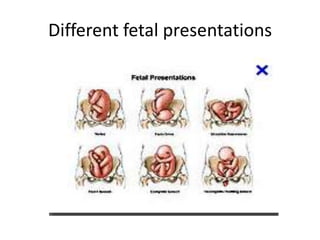
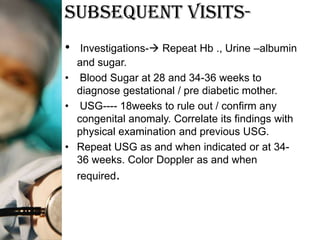
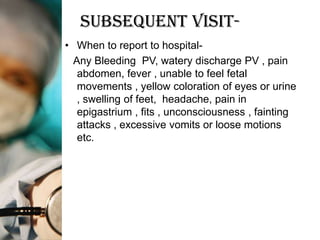
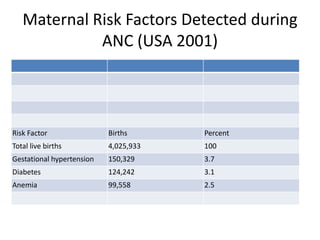
This document outlines the protocol for antenatal clinic visits. It recommends that pregnant women have at least 4 checkups - in the first, second, and third trimesters and between 36 weeks and term. The first visit includes registration, history taking, examinations, and basic investigations. Subsequent visits monitor weight, blood pressure, fetal growth and position. Investigations are repeated as needed. The protocol advises on nutrition, rest, medication, symptoms to report, and maternal risk factors identified during antenatal care.