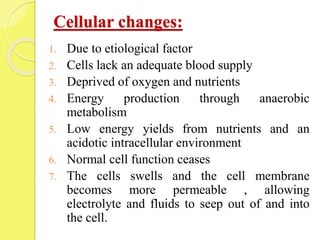
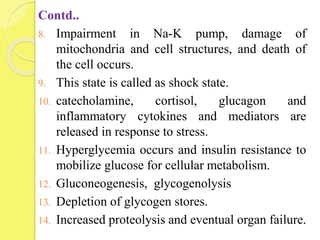
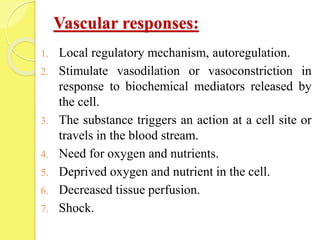
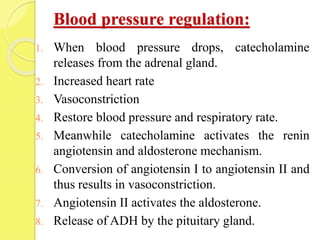
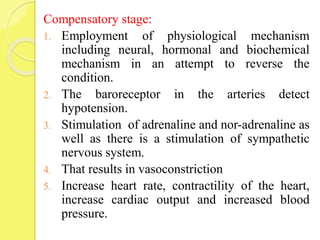
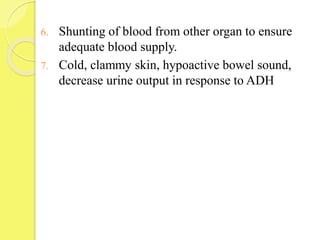
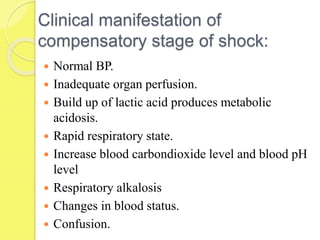
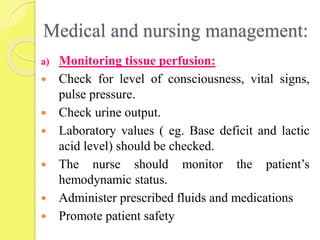
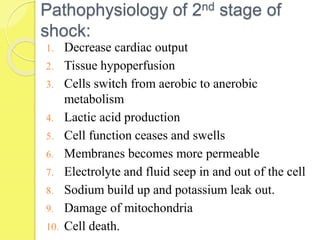
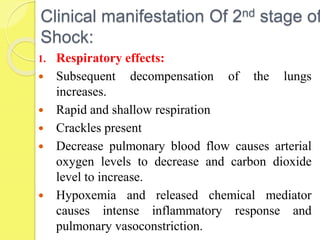
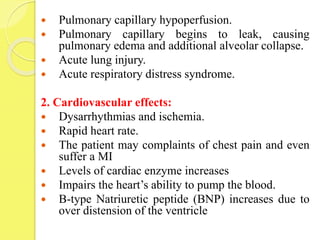
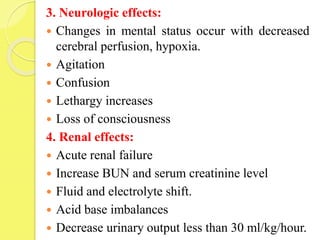
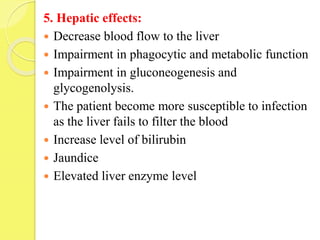
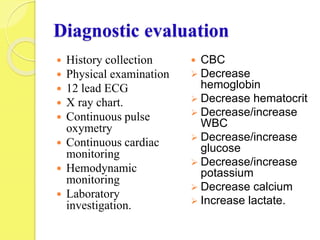
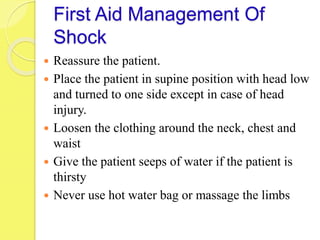
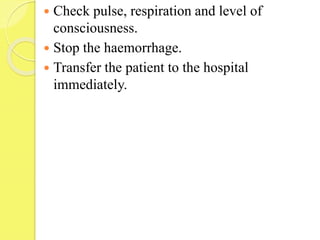
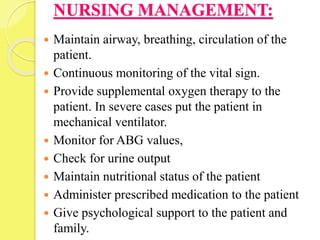
The document discusses shock, including its definition, stages, pathophysiology, signs and symptoms, and management. Shock is defined as inadequate blood flow to tissues resulting in cell death. It discusses the compensatory and progressive stages of shock, describing the body's physiological responses in each stage and associated clinical manifestations. Management involves monitoring for complications, maintaining safety, and addressing anxiety through communication and reassurance.