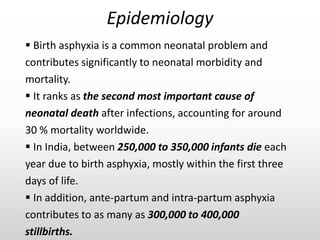
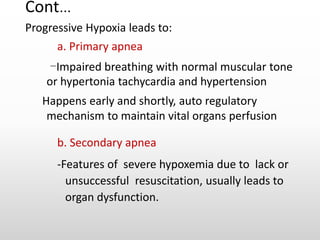
Birth asphyxia occurs when a newborn fails to breathe or has reduced oxygen delivery at birth. It is a major cause of neonatal mortality and morbidity worldwide. Risk factors include maternal infections, post-term pregnancy, fetal anomalies, and complications during delivery. The pathophysiology involves hypoxic cellular damage to vital organs like the brain. Clinical features range from mild to severe and include abnormal heart rate, breathing issues, and multi-organ involvement. Diagnosis is based on history, Apgar scores, blood tests, and neurological exam. Management involves resuscitation and treating complications, while hypothermia therapy may improve outcomes from hypoxic-ischemic encephalopathy. Outcomes depend on severity but can include death or disabilities like