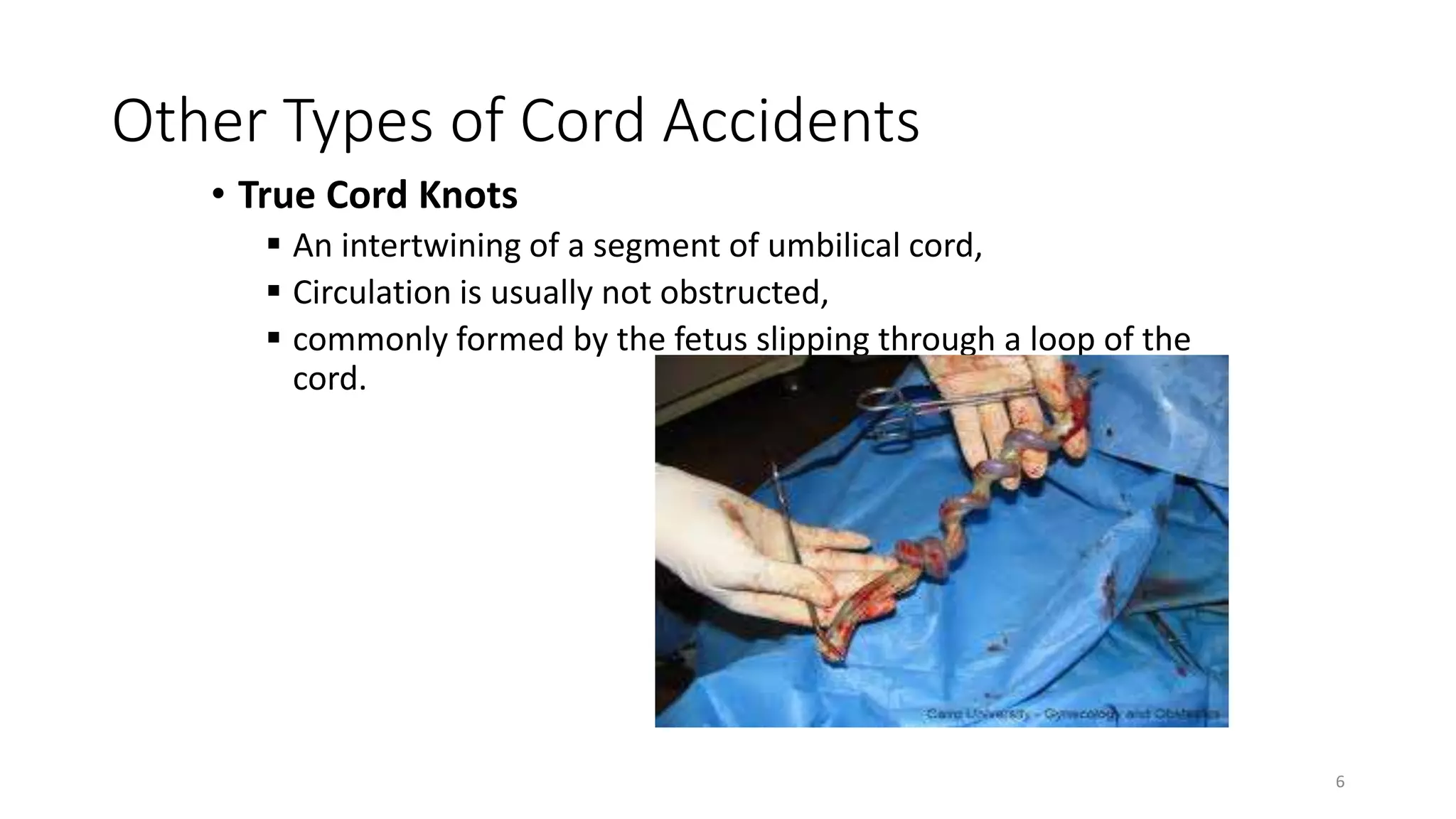
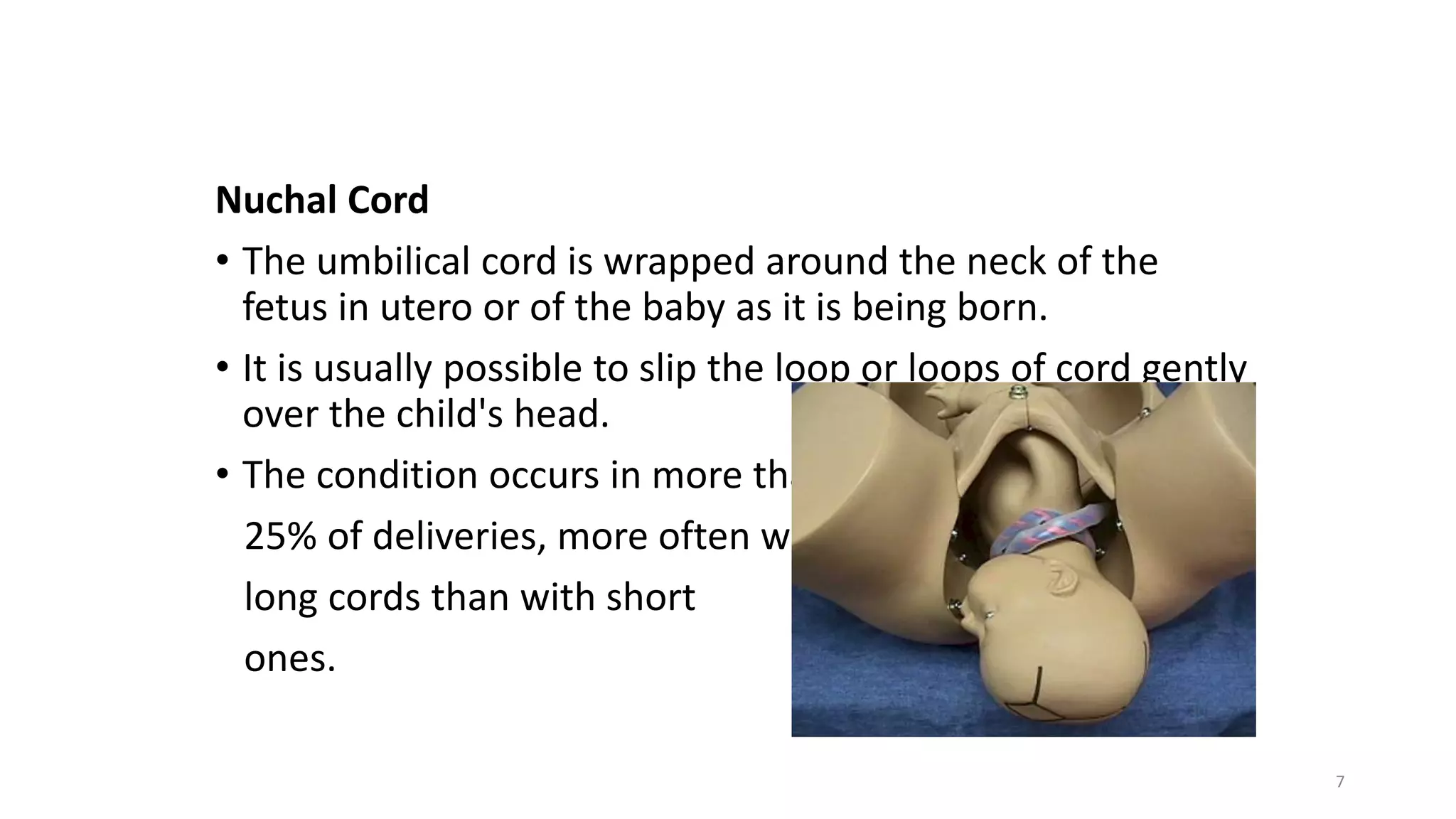
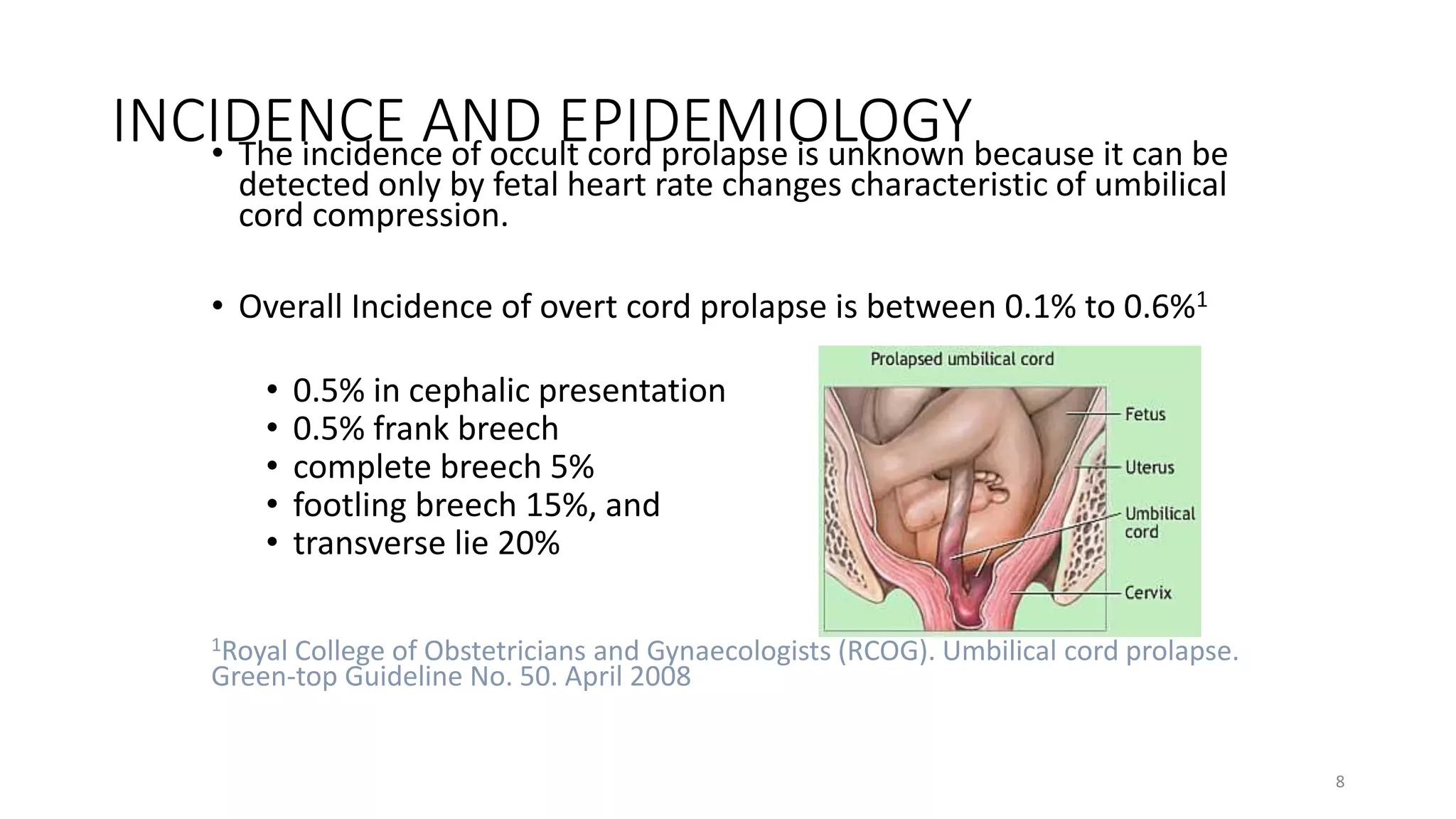
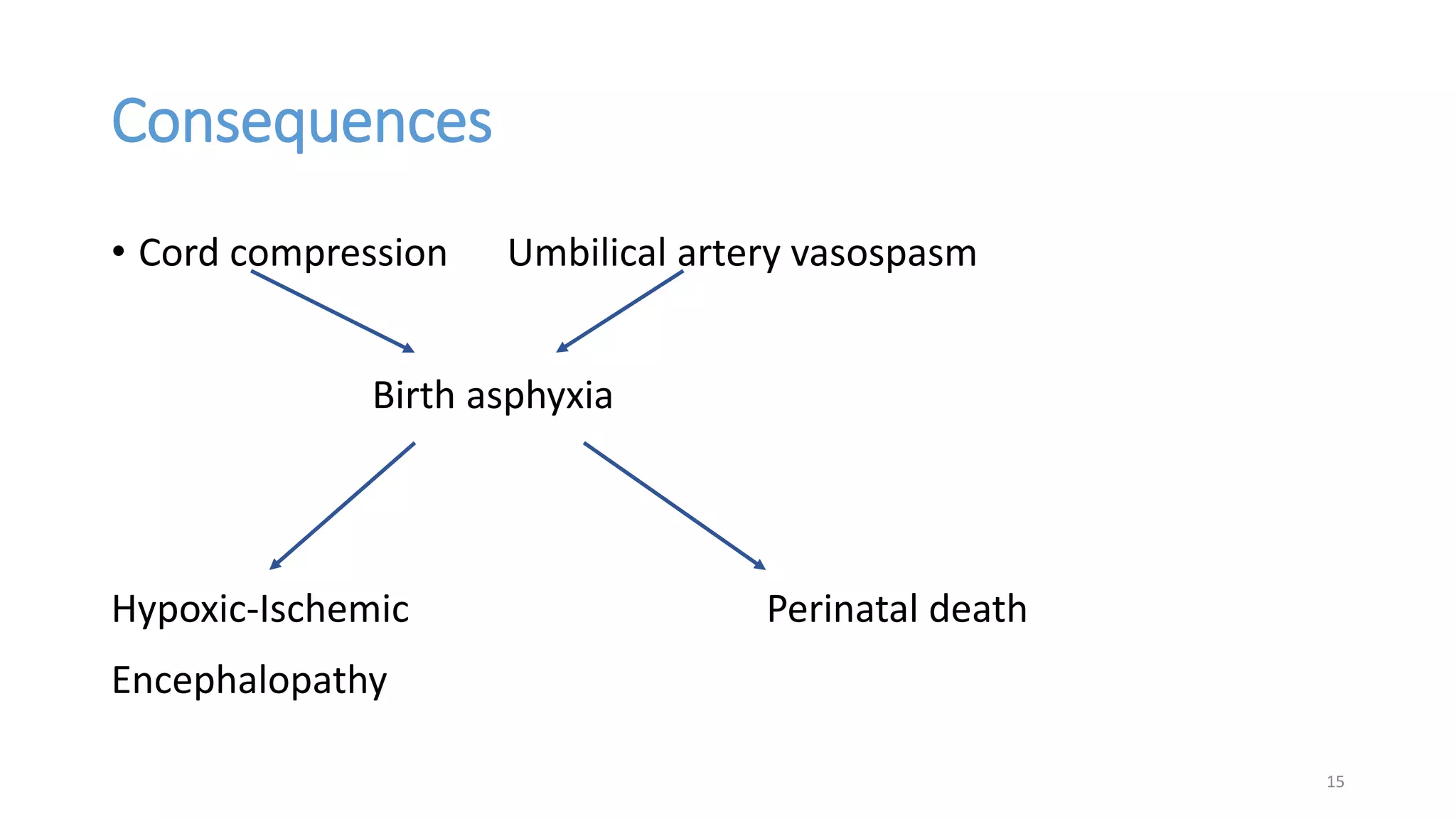
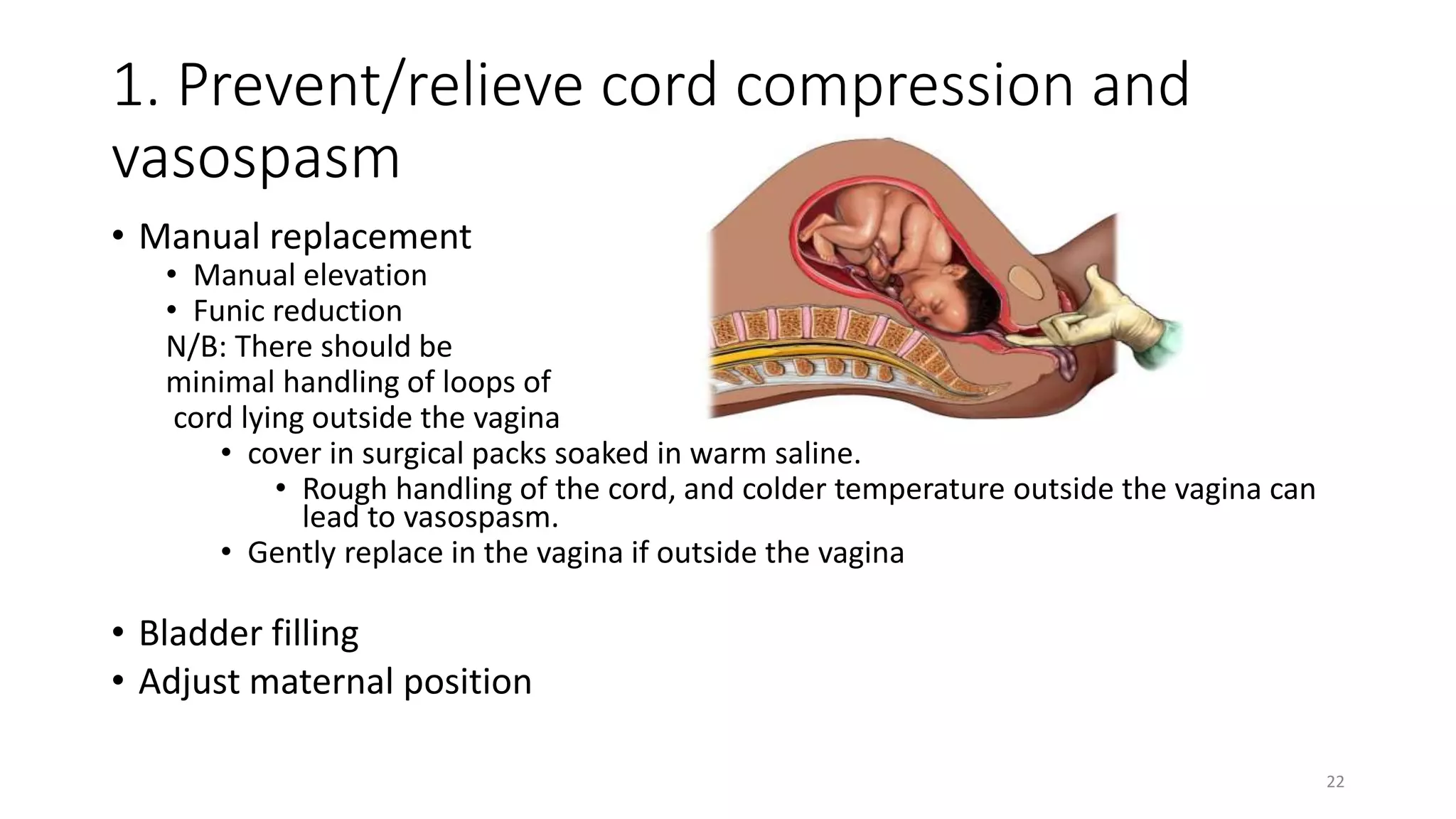
Cord prolapse is an obstetric emergency that can lead to fresh stillbirth and requires timely management, especially in developing countries where access to surgical intervention may be limited. The document outlines the definition, types, incidence, risk factors, and management strategies for cord prolapse, emphasizing the importance of early diagnosis and rapid delivery to prevent fetal distress and death. Counseling for affected women is also recommended to address potential psychological impacts following such emergencies.