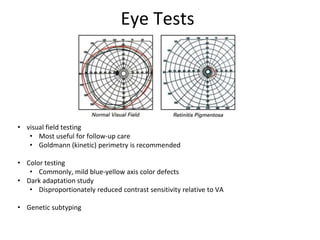
Retinitis pigmentosa (RP) is a genetic disorder affecting the retina, leading to gradual vision loss that often starts with night blindness and progresses to peripheral vision loss and ultimately blindness. Diagnosis involves various eye tests, with electroretinogram (ERG) being crucial, while management includes pharmacological treatments, surgical interventions, and emerging gene therapy and stem cell solutions. The condition varies significantly in severity and progression between individuals, particularly between males and females.












![gene therapy
• under investigation
• to replace the defective protein by using DNA vector (eg, adenovirus, lentivirus)
• Gene therapy was successful in providing the missing protein to a dog with Leger congenital
amaurosis (LCA)
• adeno-associated virus (AAV)
• Briard dog with RPE65 mutations after treatment had 20% of its RPE cells express the
functional protein, thereby allowing the dog to see
• also effective in a mouse model of Leber congenital amaurosis
• Trials have also begun for RP, although currently only for MERTK gene mutation
• problems : wide heterogeneity of defects in RP
• Jacobson et al found that gene therapy is acceptably safe and effective in the extrafoveal retina for
LCA caused by RPE65 mutations; however, no benefit and some risk was noted in treating the fovea.
Age-dependent effects were not evident.[18]
• It is not known which, if any, of the RP forms will show reversibility (even with a nondestructive
reinsertion of the appropriate gene in the appropriate locus with appropriate regulation).](https://image.slidesharecdn.com/nw2016rp02-160831013222/85/Nw2016-retinitis-pigmentosa-16-320.jpg)

