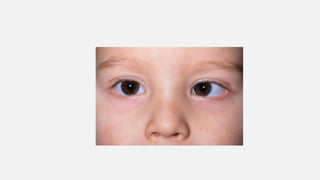
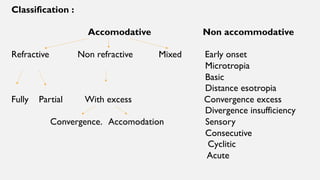
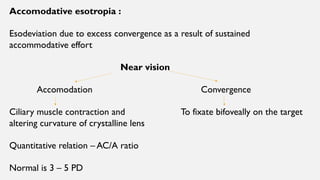
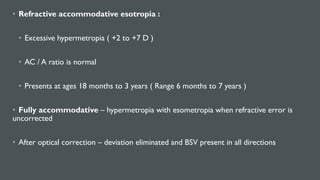
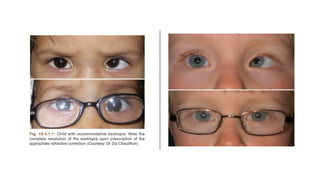
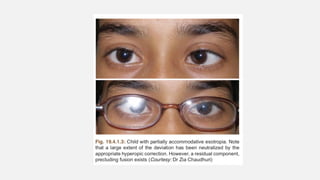
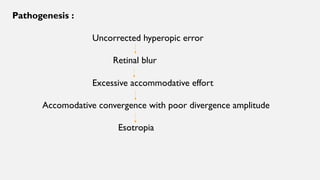
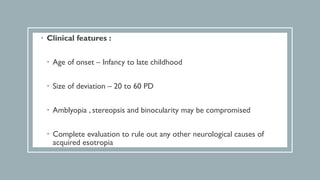
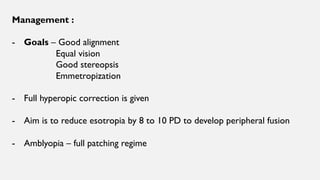
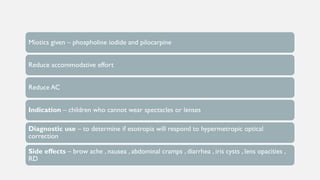
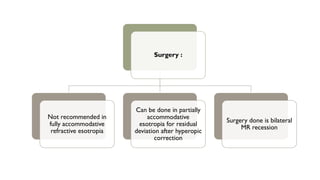
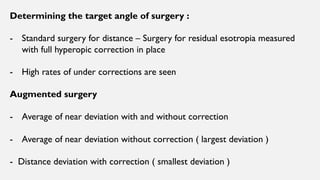
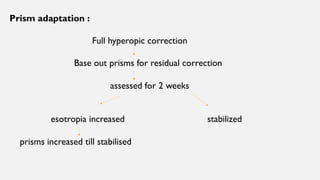
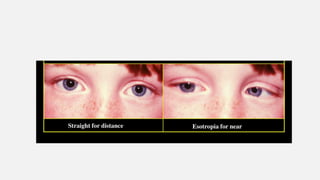
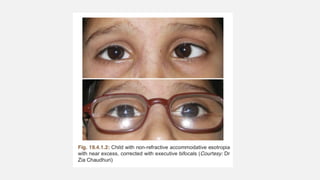
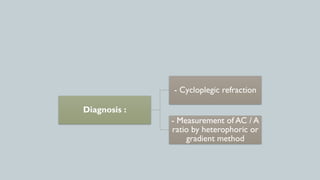
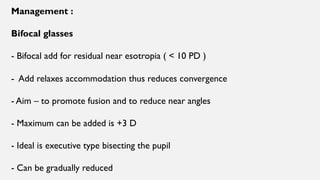
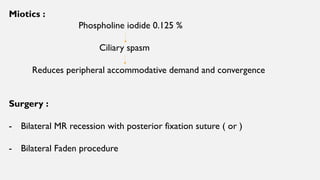
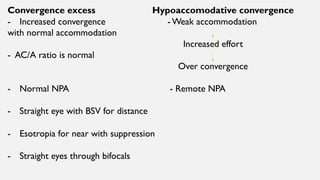
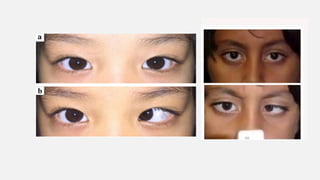
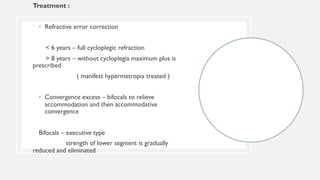
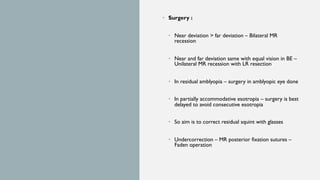
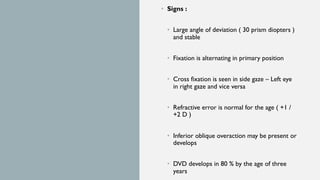
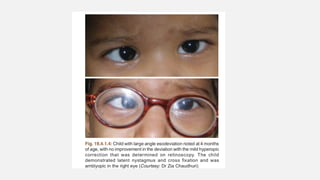
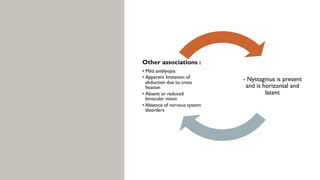
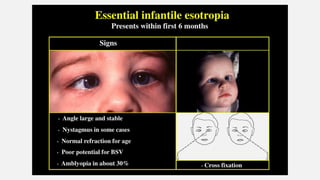
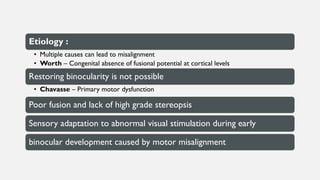
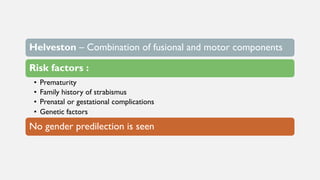
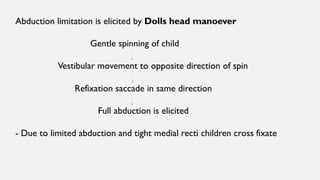
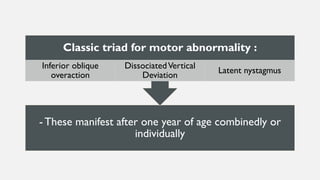
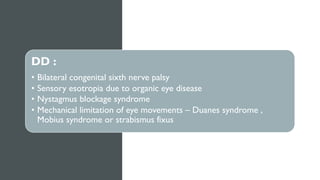
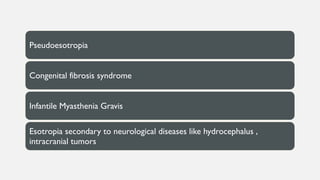
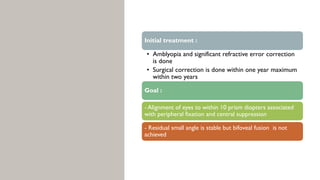
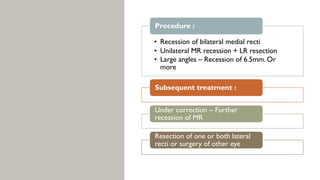
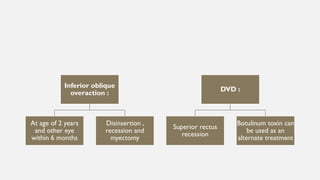
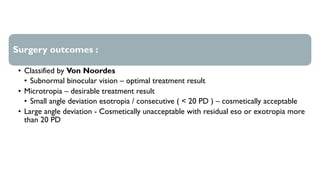
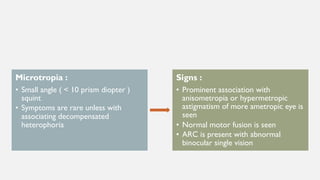
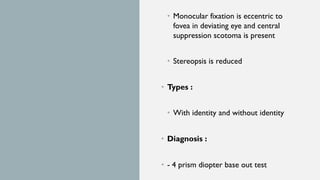
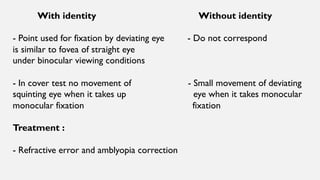
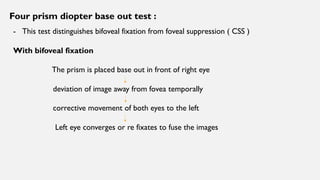
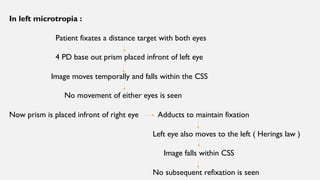
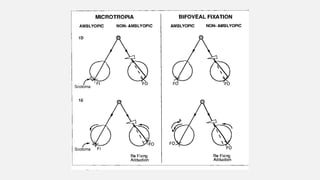
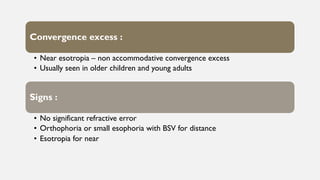
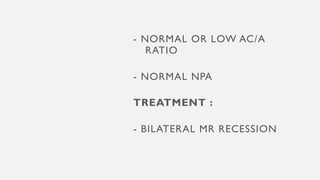
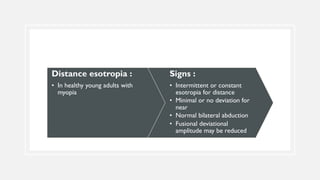
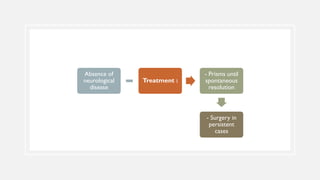
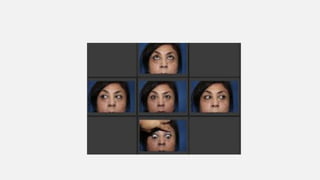
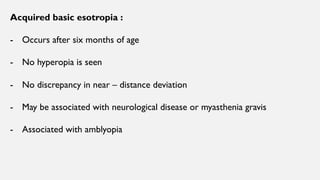
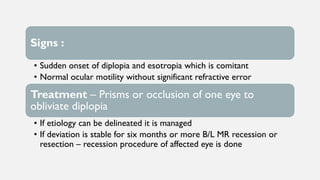
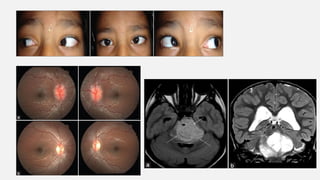
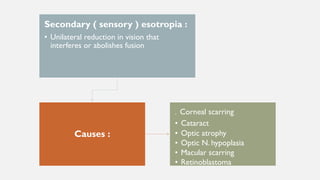
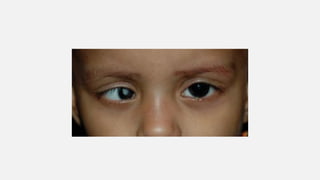
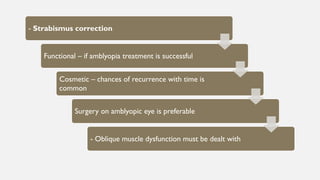
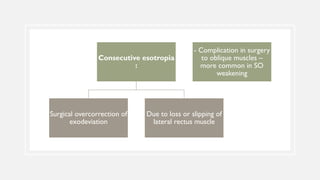
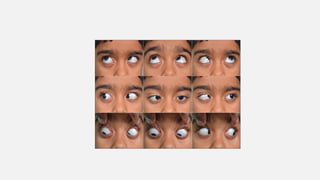
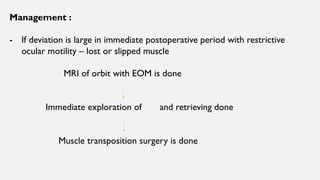
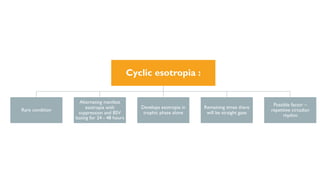
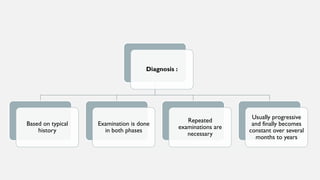
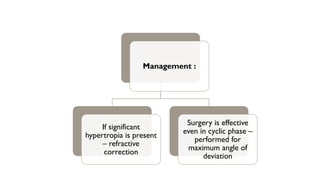
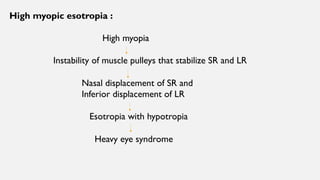
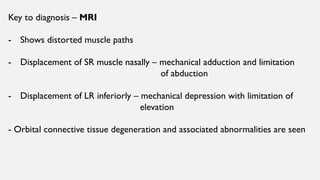
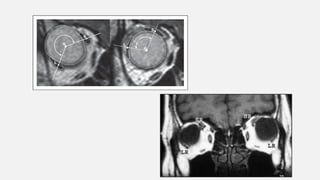
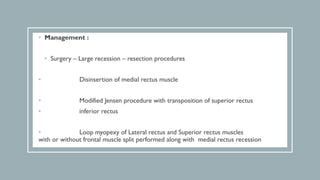
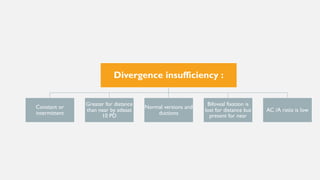
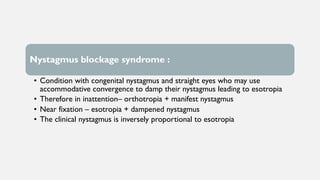
This document discusses esotropia, or inward eye deviation. It defines concomitant and inconcomitant esotropia and describes various types including accommodative, refractive, and early onset esotropia. Accommodative esotropia is caused by excess convergence during accommodation. Refractive accommodative esotropia involves excessive hyperopia. Early onset esotropia develops within 6 months and involves a large, stable deviation. The document outlines signs, etiologies, and management including optical correction, miotics, and surgery for different types of esotropia.