The document discusses several vascular and hereditary retinal diseases:
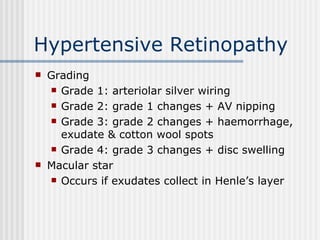
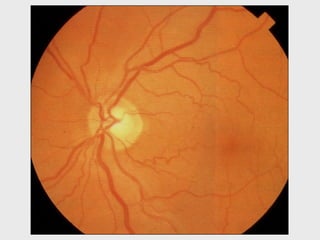
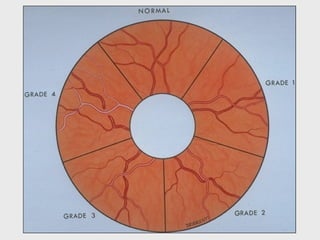
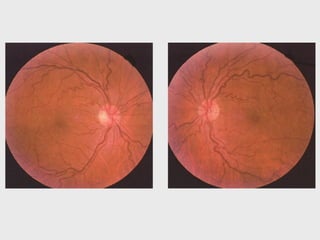
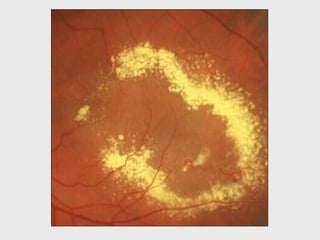
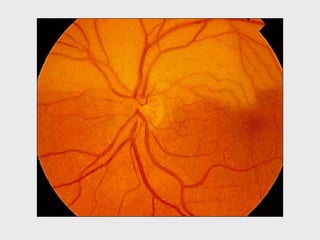
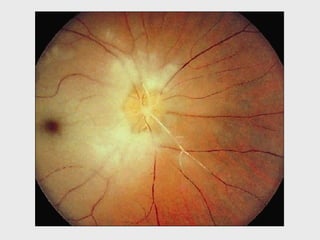
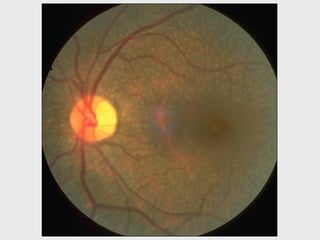
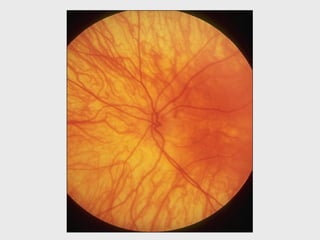
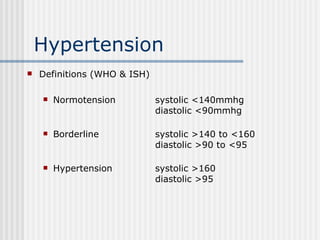
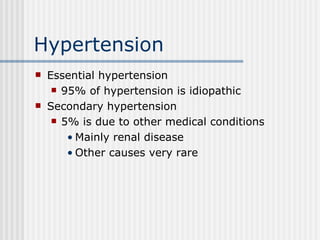
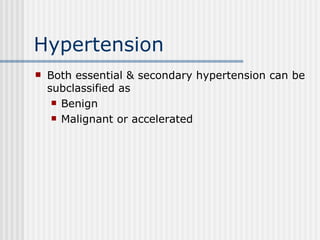
1. Hypertension affects 15-20% of the population and can lead to complications like ischemic heart disease if not properly treated. Retinal findings in hypertensive retinopathy include arteriolar changes and hemorrhages.
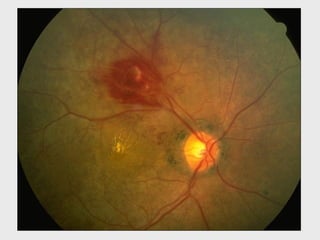
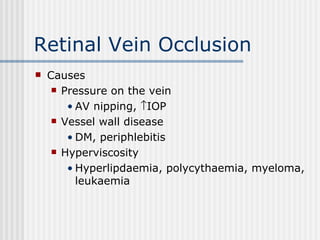
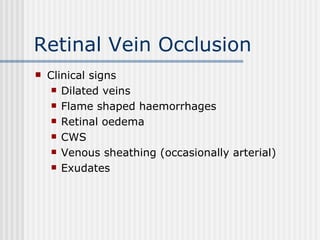
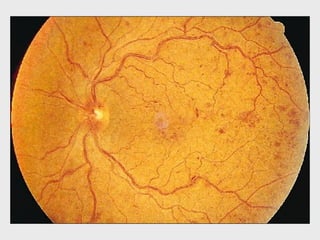
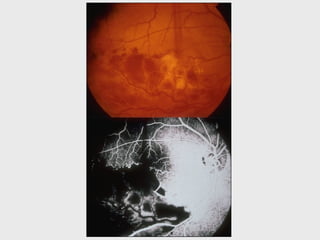
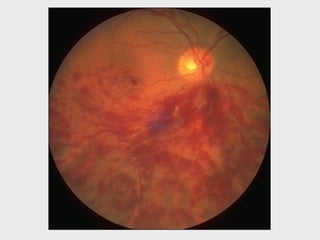
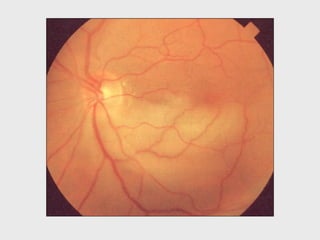
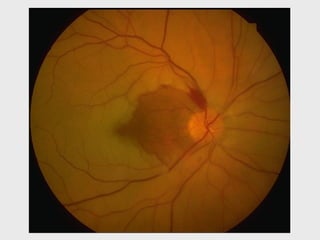
2. Retinal vein occlusion is caused by pressure on the retinal veins and presents with dilated veins, flame-shaped hemorrhages, and retinal edema.
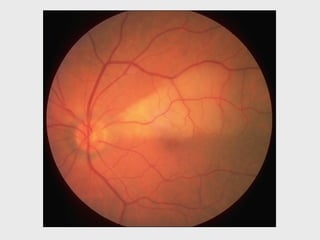
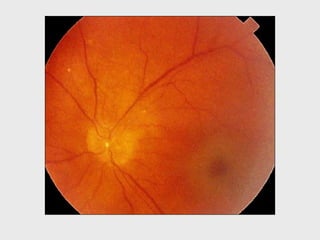
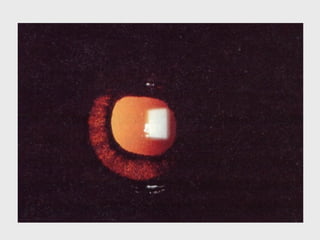
3. Retinal artery occlusion typically results from emboli and presents with sudden vision loss and a cherry red spot at the macula.
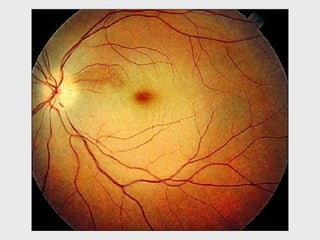
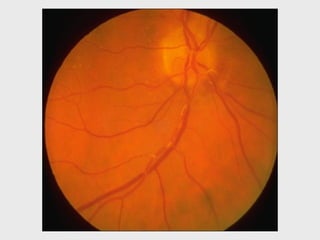
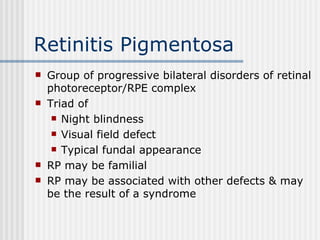
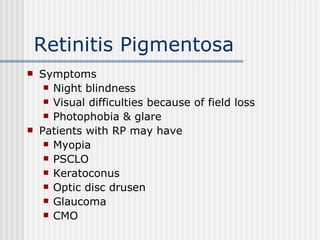
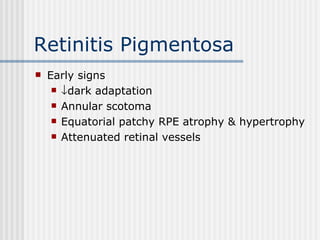
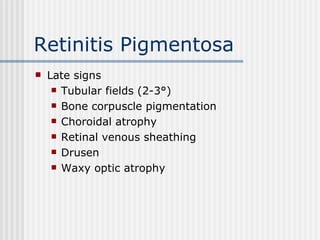
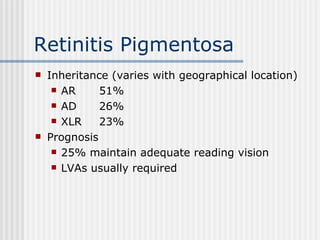
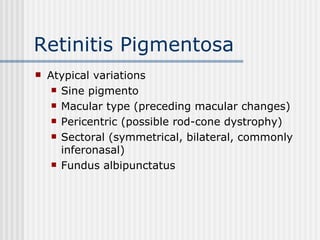
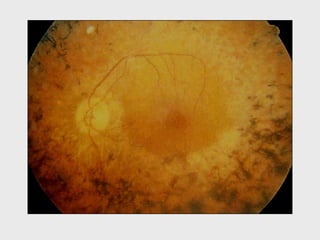
4. Retinitis pigmentosa is a group of inherited retinal diseases characterized by night blindness, visual
![Hypertension The spectrum of hypertensive eye disease [Arteriosclerotic retinopathy] Hypertensive retinopathy CRVO/BRVO CRAO/BRAO AION Cranial neuropathies](https://image.slidesharecdn.com/hpptfilesbradfordresourcesoculardiseaselecture08-090317003123-phpapp01/85/VASCULAR-AND-HEREDITARY-RETINAL-DISEASE-6-320.jpg)