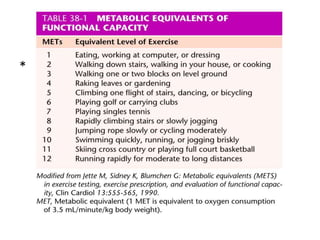
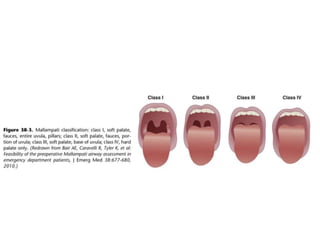
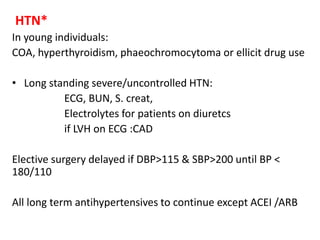
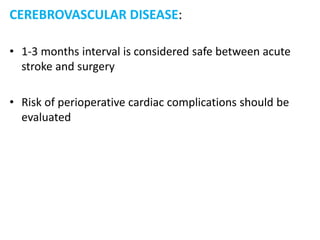
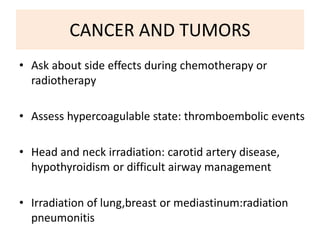
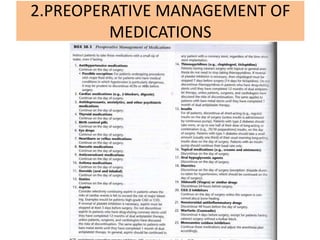
This document provides an overview of preanesthesia evaluation. The key purposes are to obtain relevant medical history, assess perioperative risks, order appropriate tests, and formulate an anesthetic plan. Important components of the medical history include past and current medical problems, medications, allergies, and lifestyle factors. A physical exam focuses on vital signs, airway assessment, and systemic examination. For patients with cardiovascular or pulmonary diseases, specific evaluations and tests are recommended to optimize management and identify high-risk patients. The preanesthesia evaluation aims to detect underlying conditions, evaluate perioperative risks, and develop a customized anesthetic plan tailored to each patient's needs.