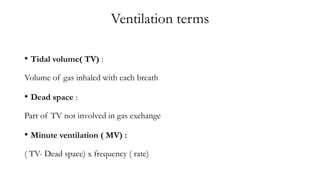
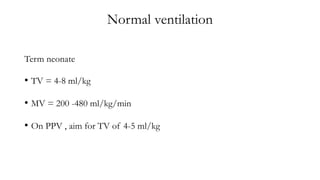
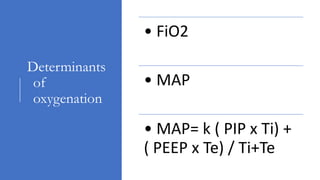
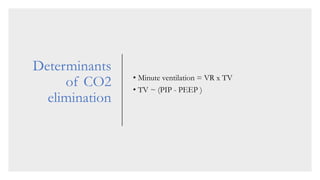
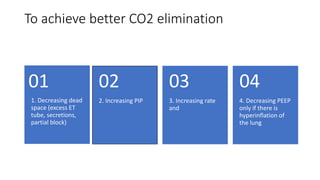
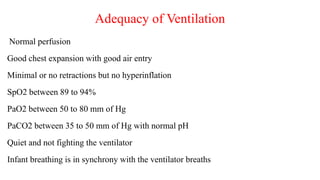
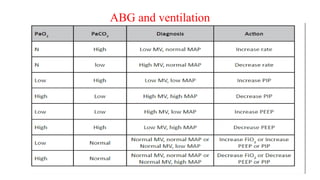
1. Ventilation involves delivering gas to the lungs at an appropriate tidal volume, minute ventilation, and oxygen concentration to ensure adequate oxygenation and carbon dioxide elimination.
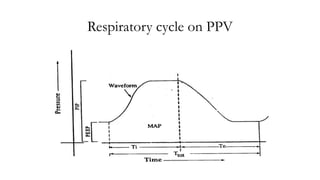
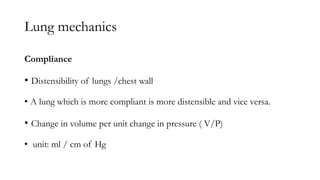
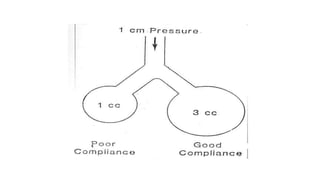
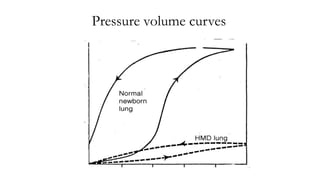
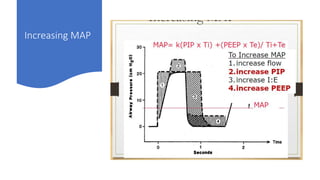
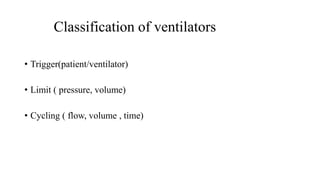
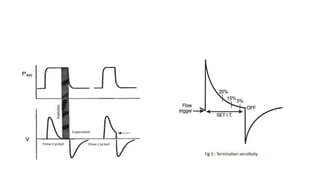
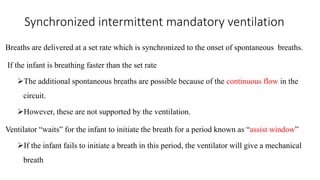
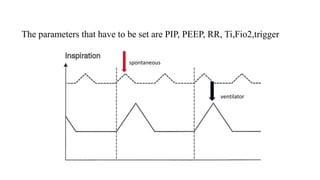
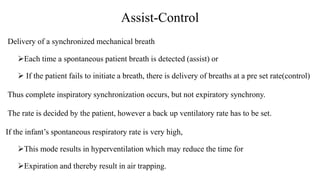
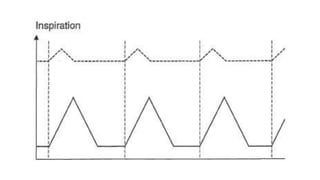
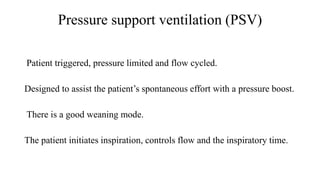
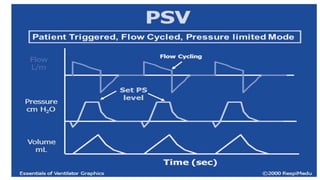
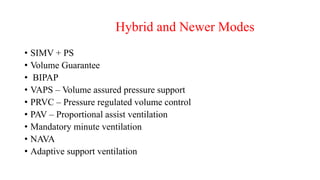
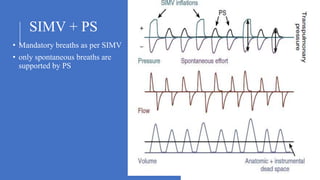
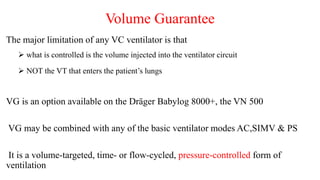
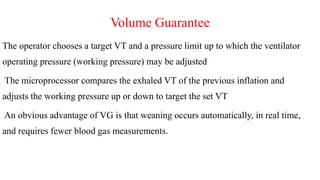
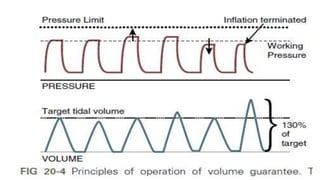
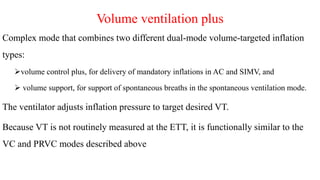
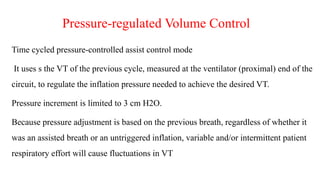
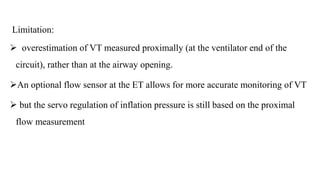
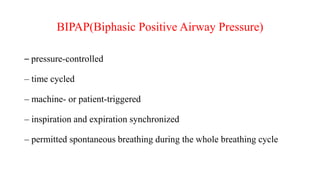
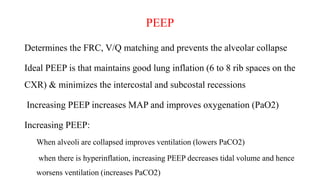
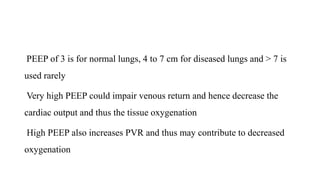
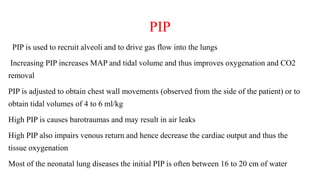
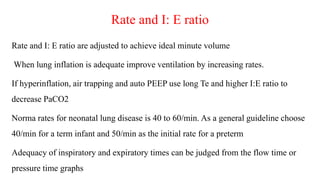
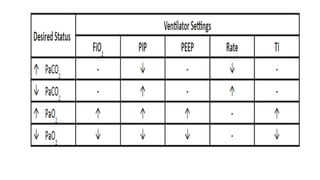
2. Various modes of ventilation include pressure-triggered modes like SIMV and pressure support ventilation as well as newer hybrid modes that combine features. Parameters like PIP, PEEP, rates and triggers must be optimized.
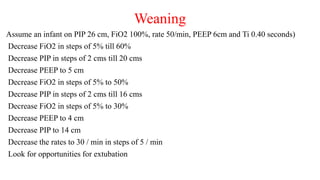
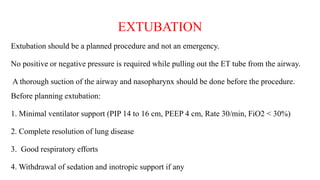
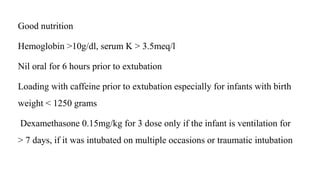
3. Weaning from ventilation requires gradually reducing support by lowering PIP, PEEP and FiO2 while monitoring blood gases to ensure adequate oxygen and carbon dioxide levels are maintained before considering extubation.