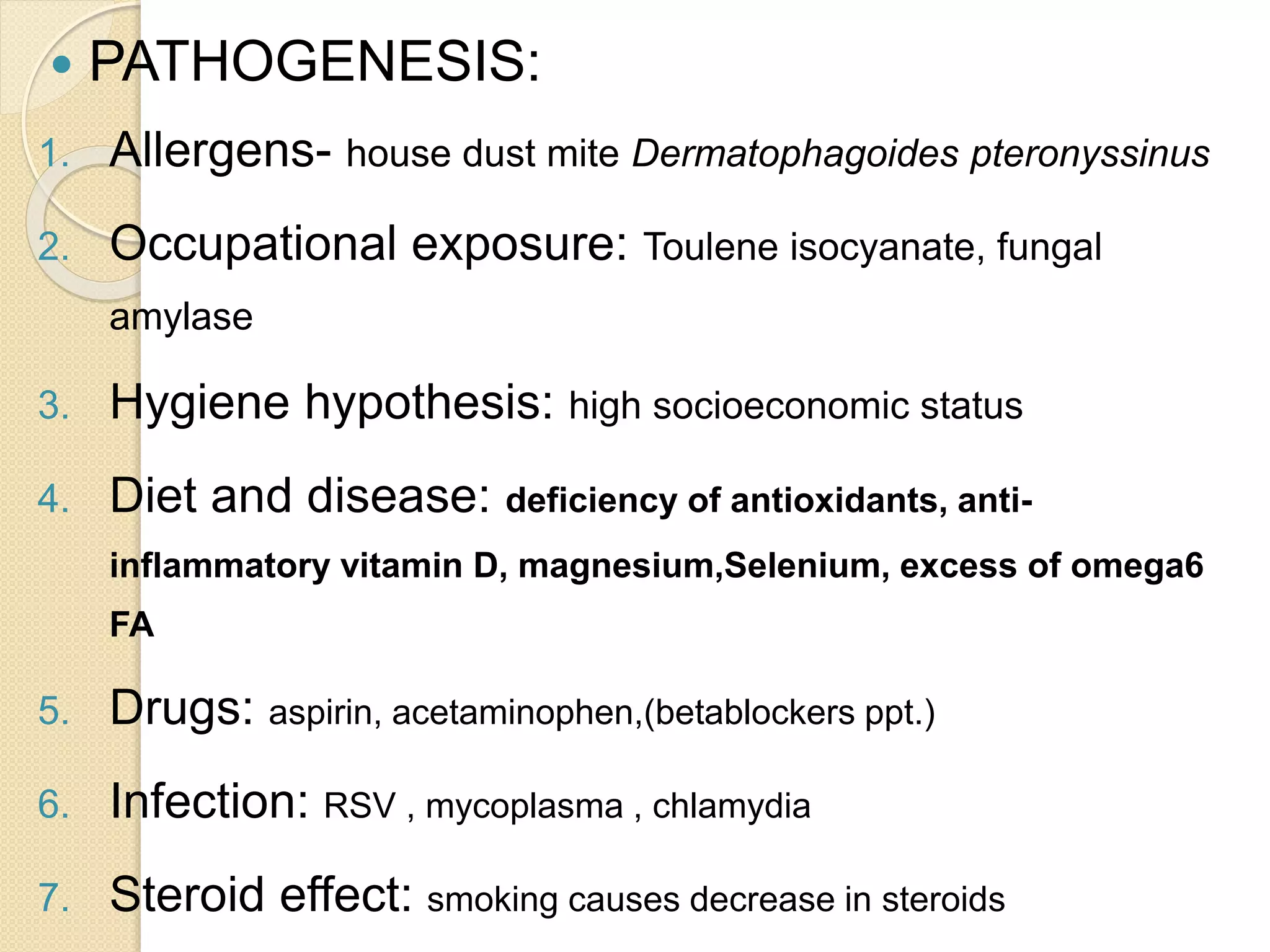
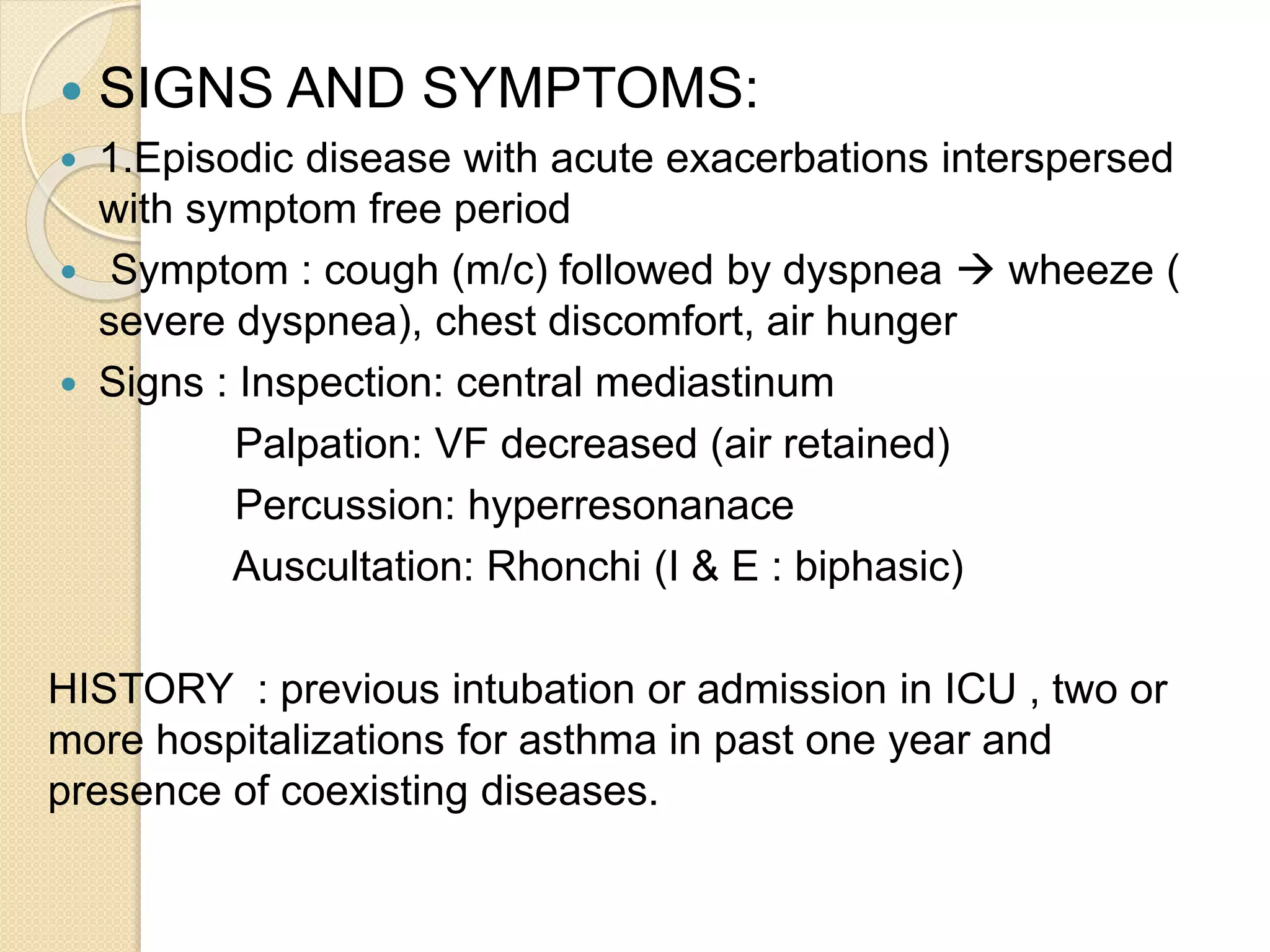
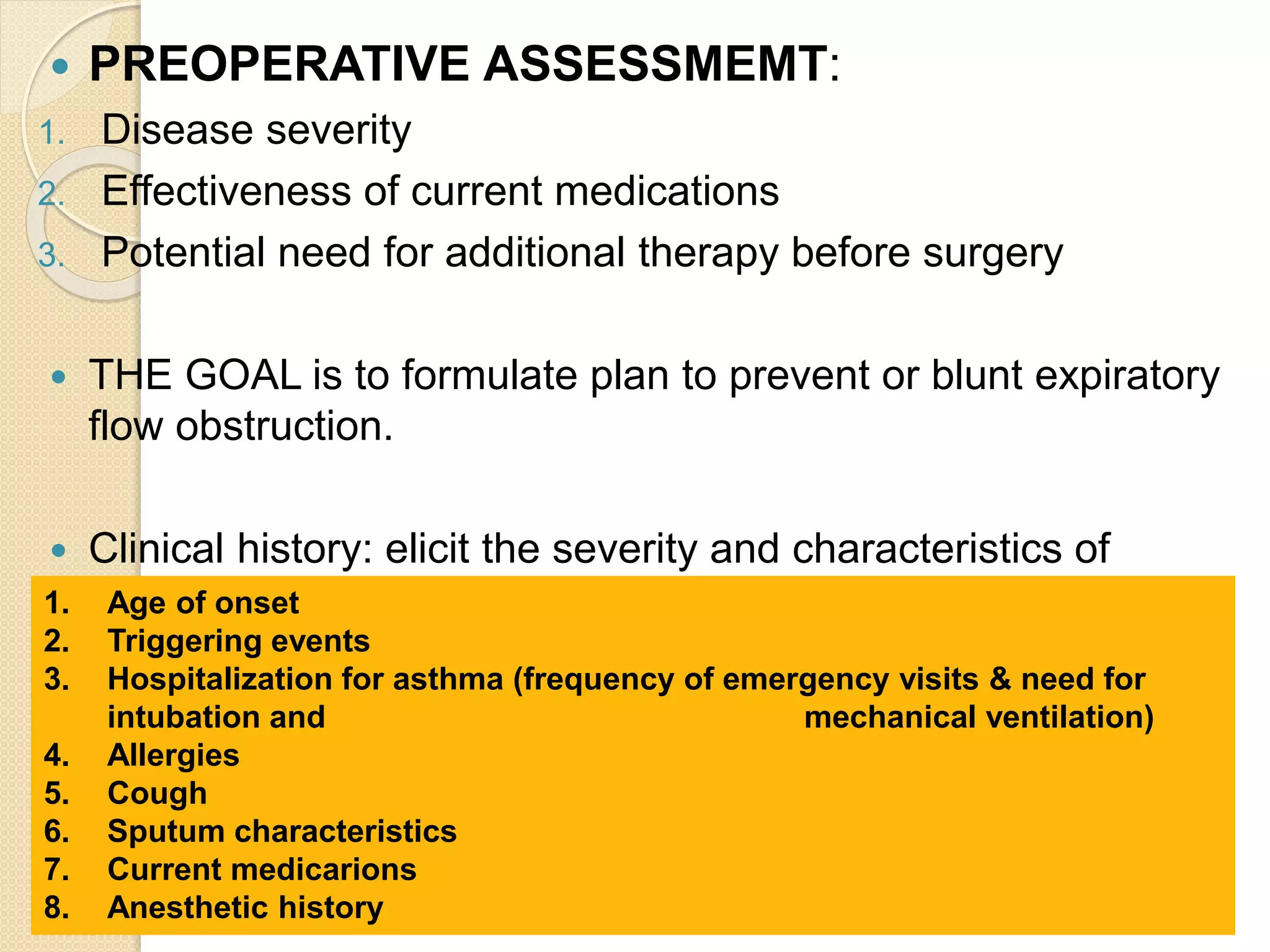
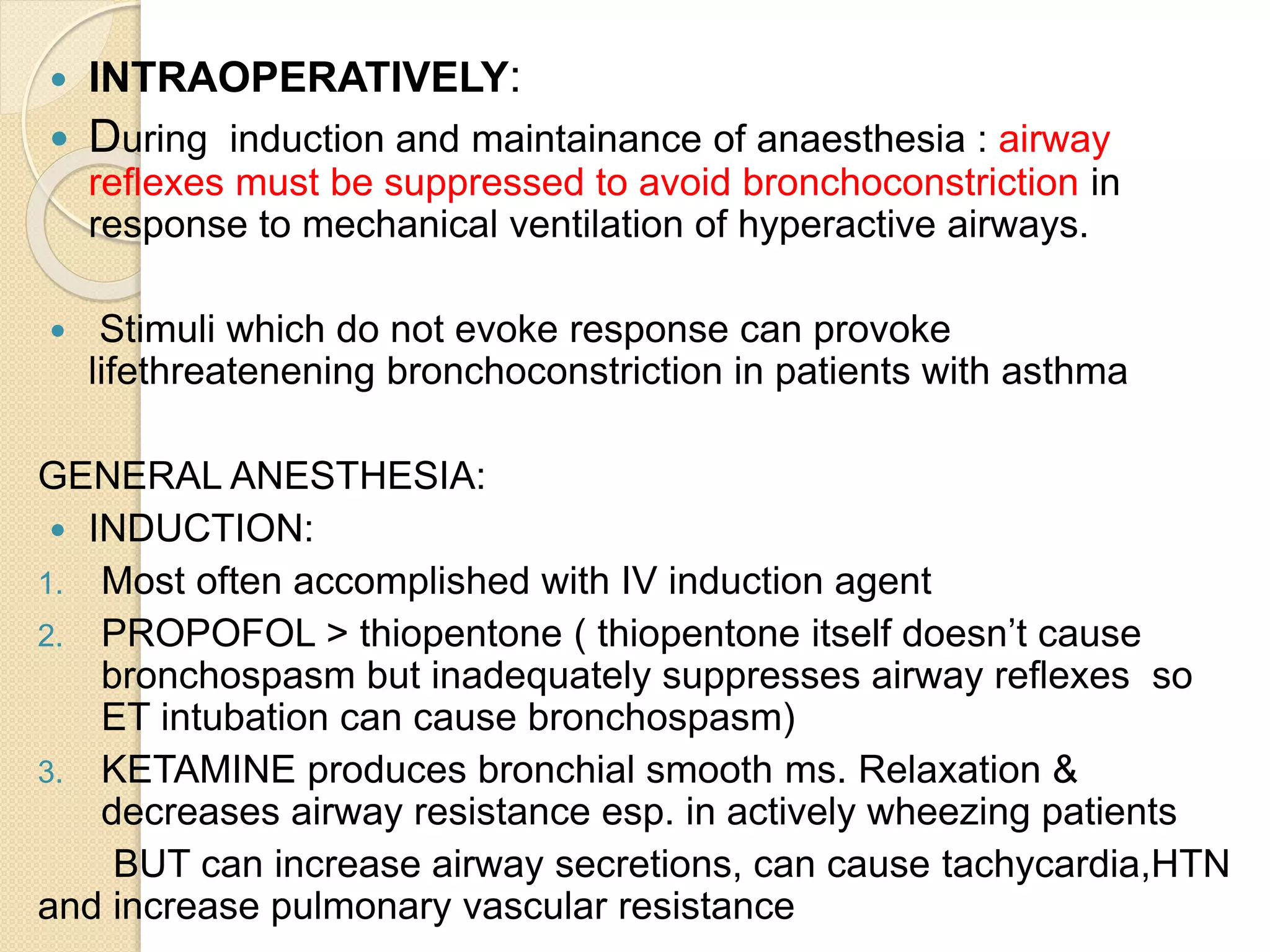
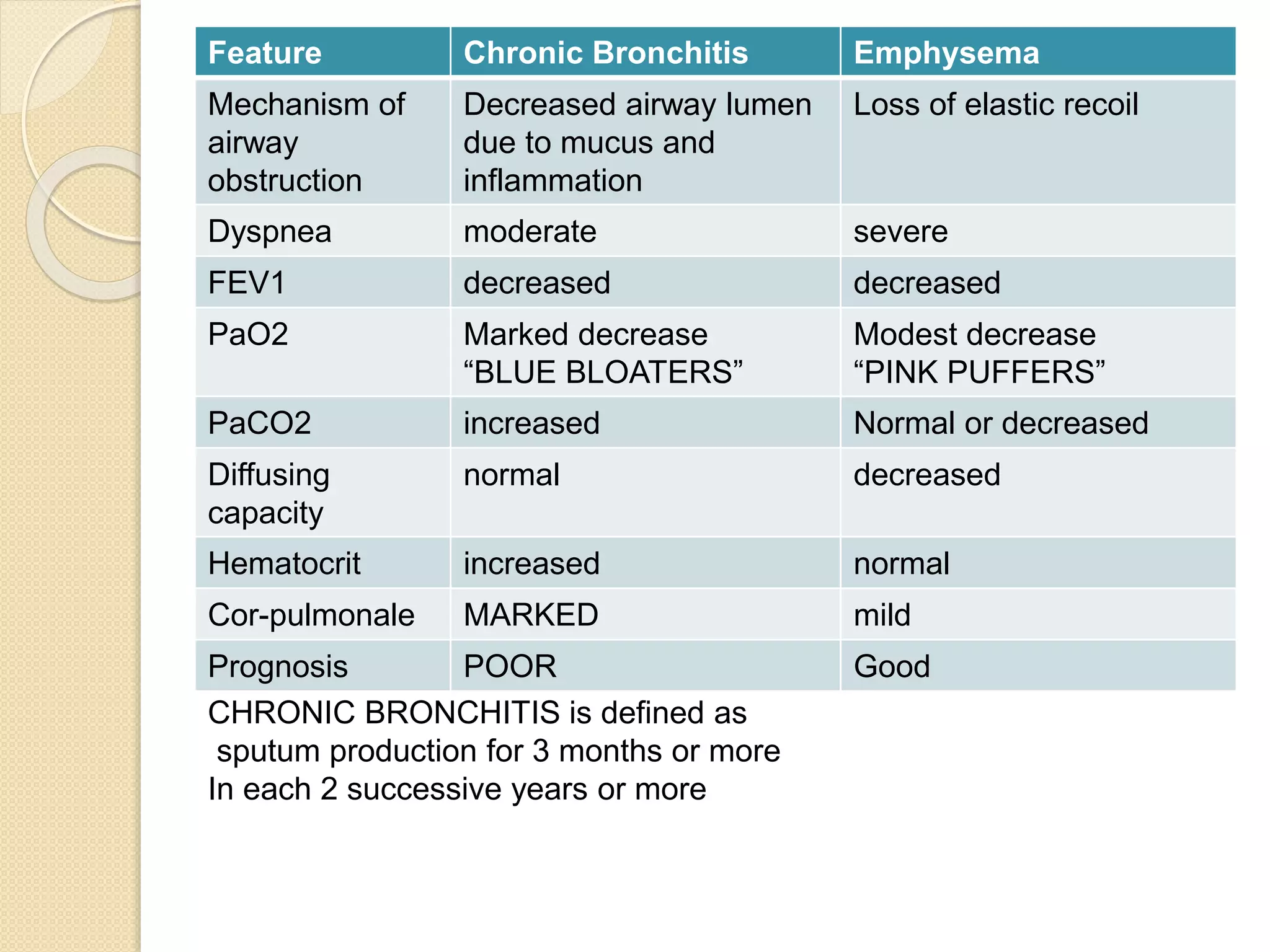
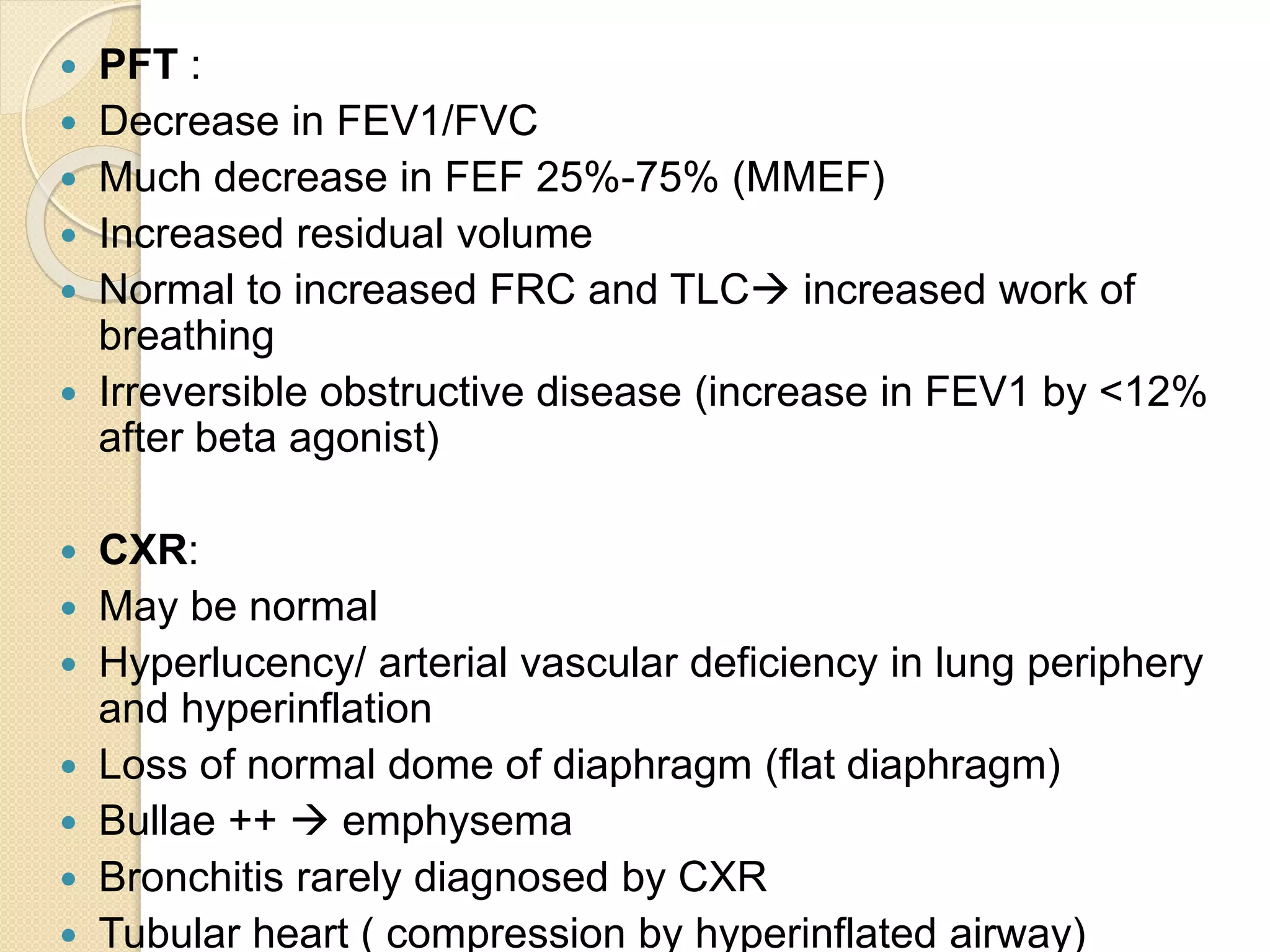
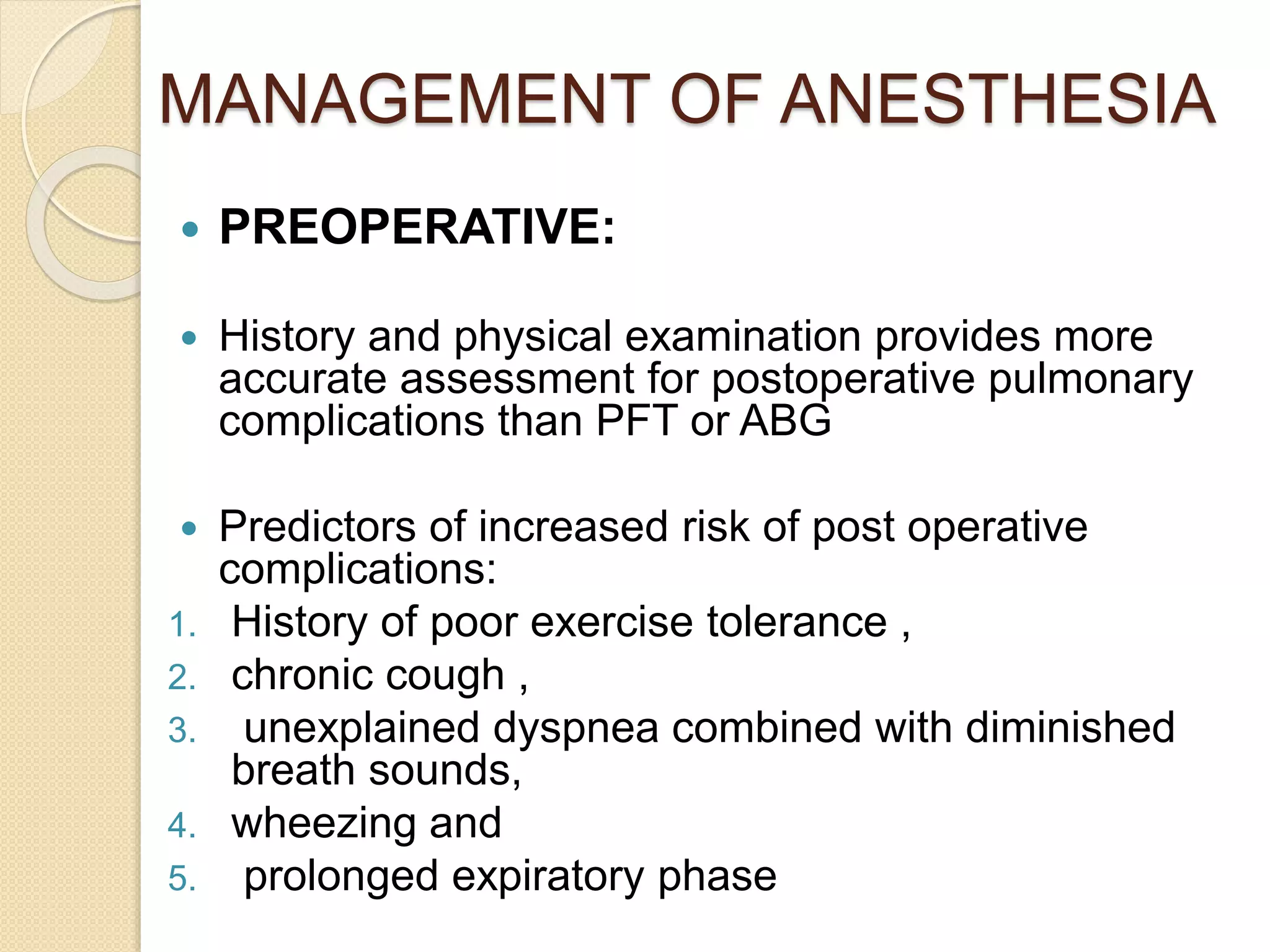
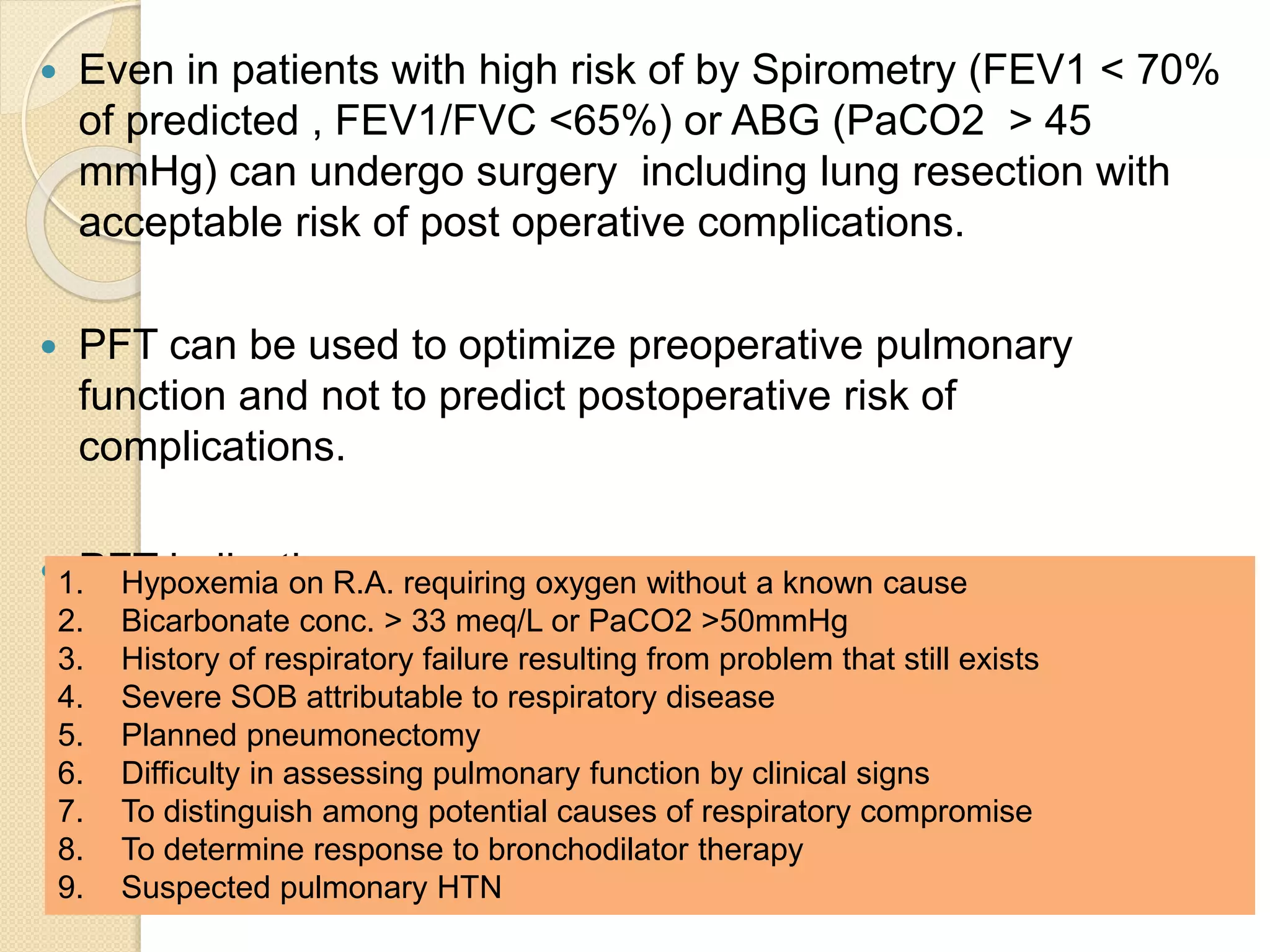
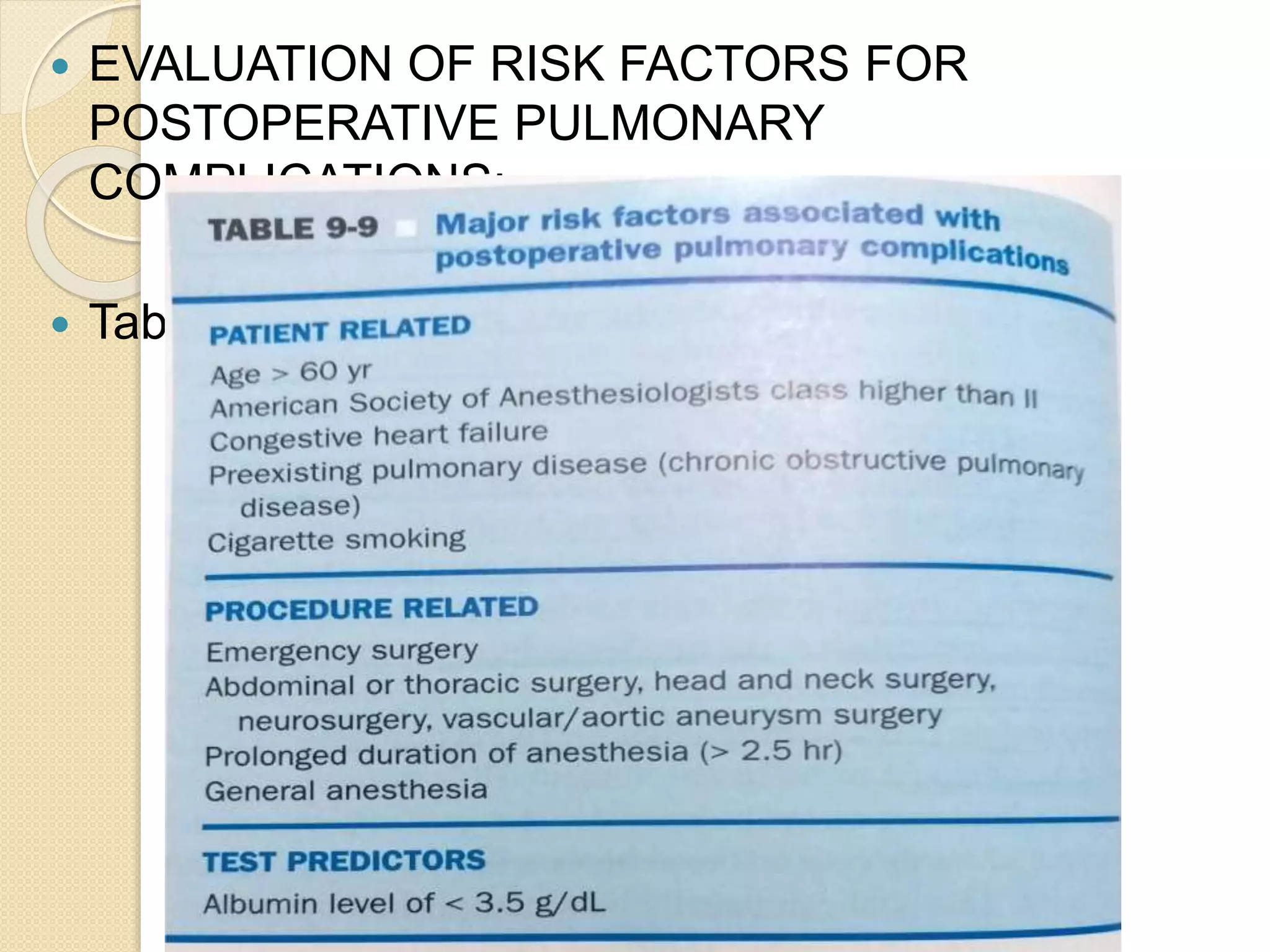
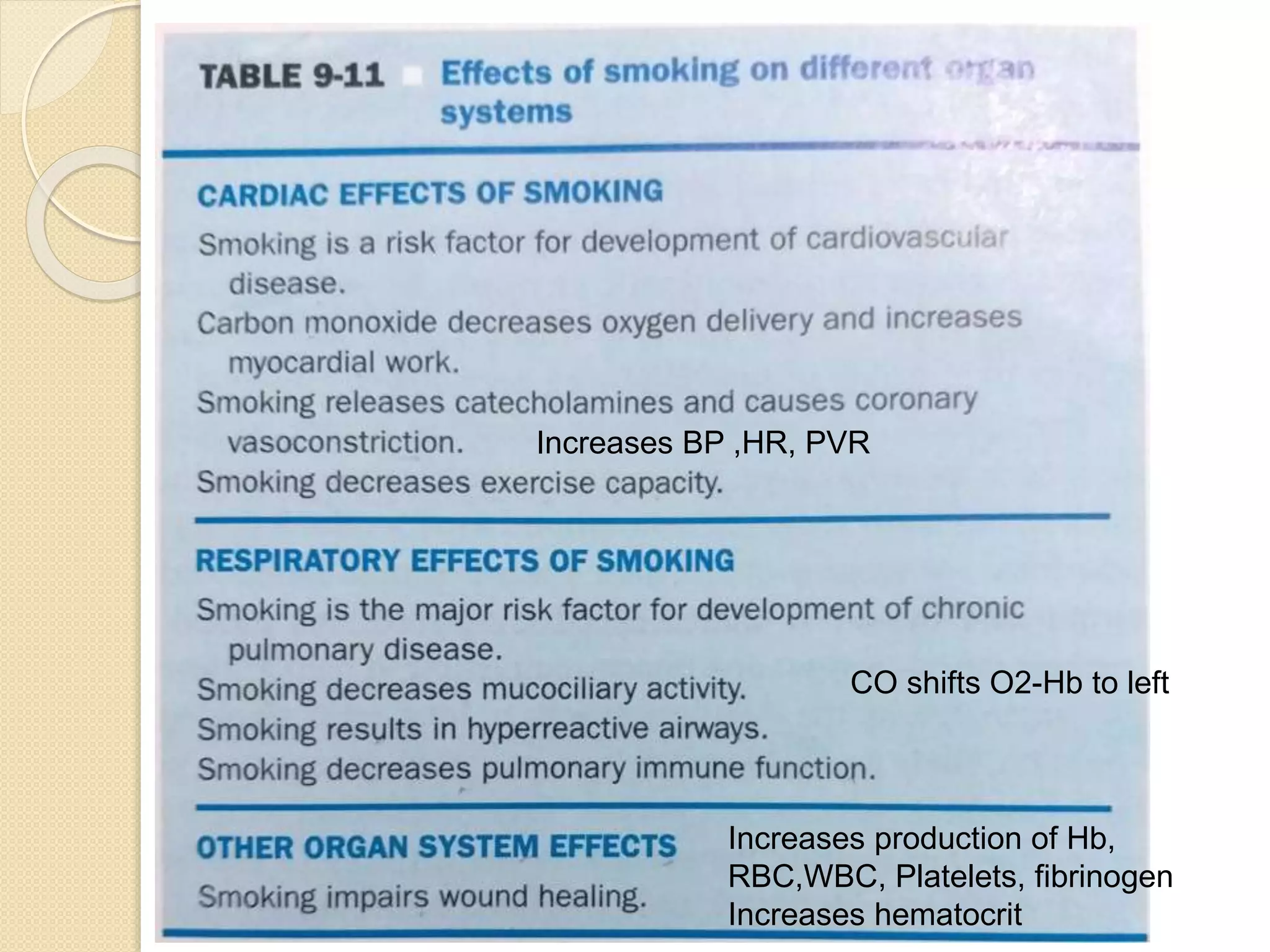
Bronchial asthma and COPD are chronic respiratory conditions characterized by airway inflammation and obstruction. Bronchial asthma involves reversible airflow limitation due to bronchospasm while COPD involves irreversible airflow limitation from lung damage. Key differences are that asthma typically presents earlier in life and has a family history, while COPD is mainly caused by smoking. Preoperative treatment aims to prevent bronchospasm during anesthesia and surgery by optimizing lung function and suppressing airway reflexes.