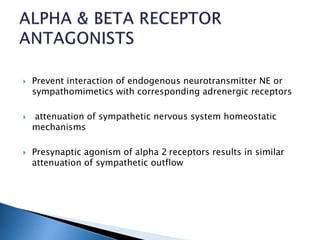
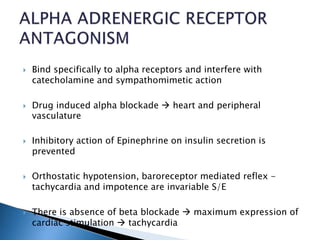
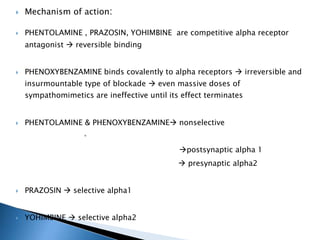
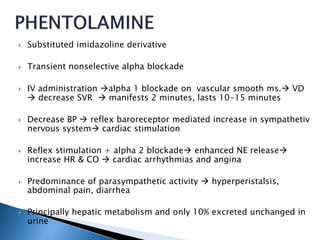
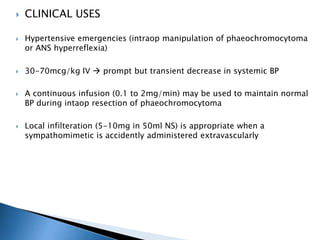
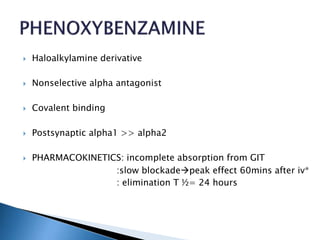
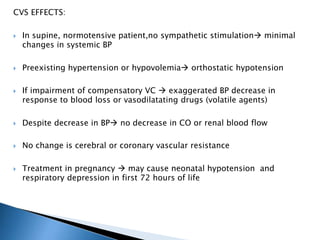
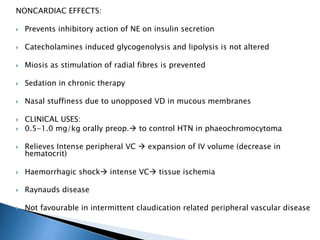
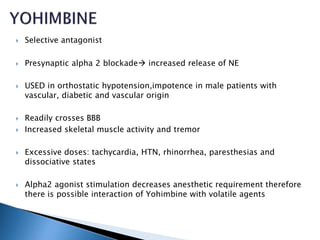
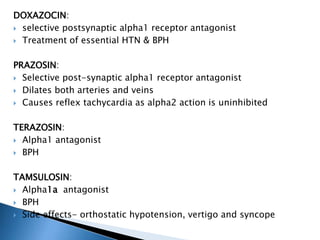
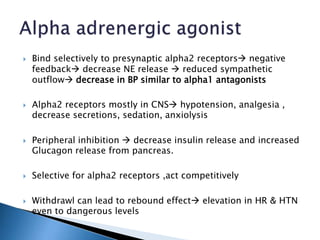
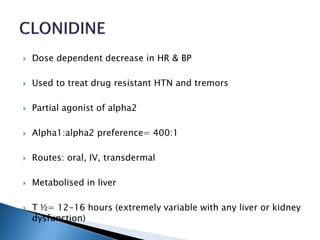
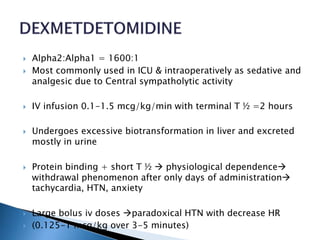
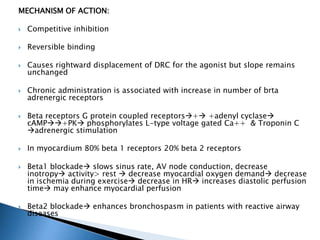
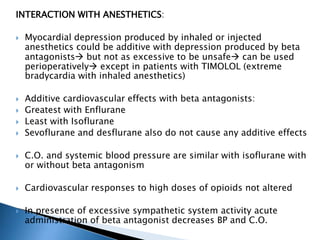
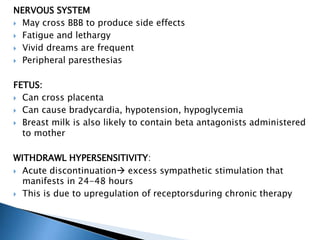
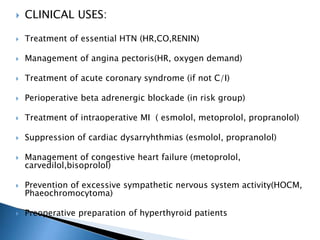
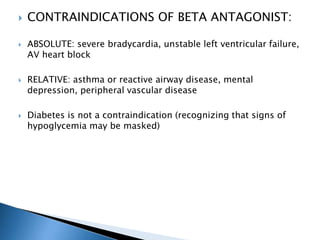
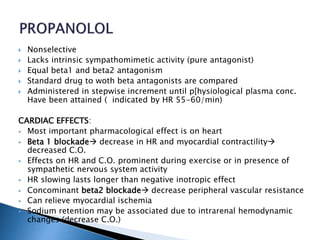
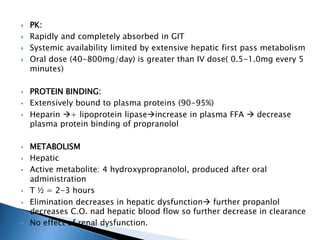
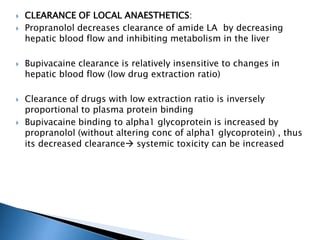
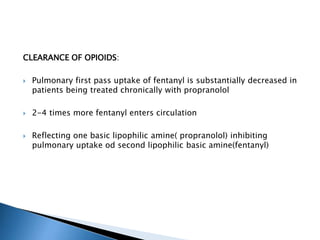
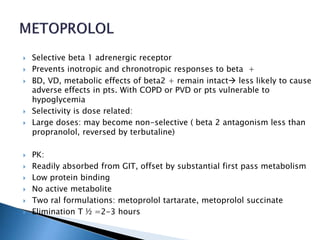
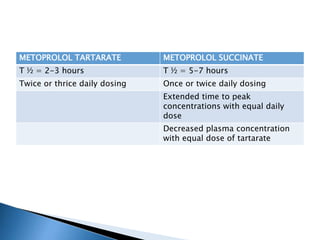
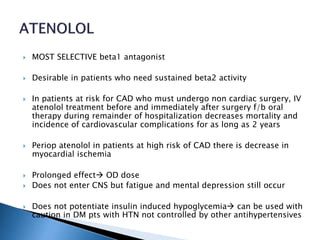
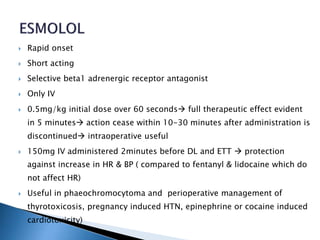
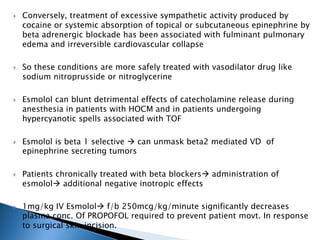
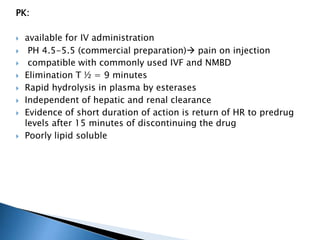
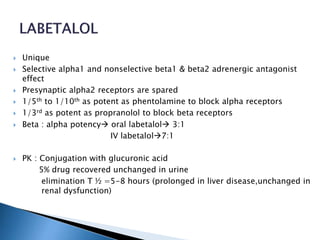
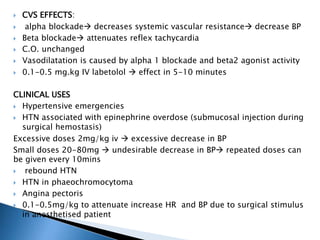
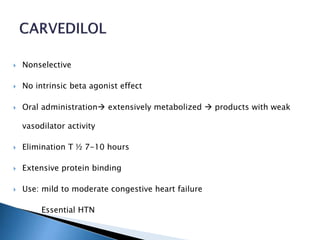
This document discusses various alpha and beta receptor antagonists. It provides details on their mechanisms of action, pharmacokinetics, clinical uses and side effects. Regarding alpha antagonists, it describes how they bind to alpha receptors to block catecholamine and sympathomimetic action. It also explains the differences between selective and non-selective alpha1 and alpha2 antagonists. For beta antagonists, it outlines their competitive inhibition of beta receptors and categorizes drugs as non-selective or cardioselective. The document discusses cardiovascular, respiratory, metabolic and other effects of both classes of drugs.