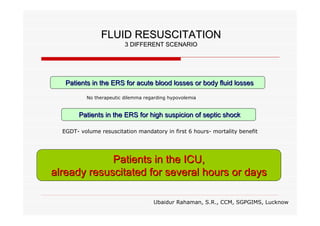
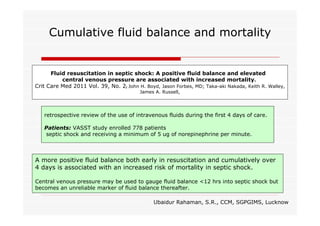
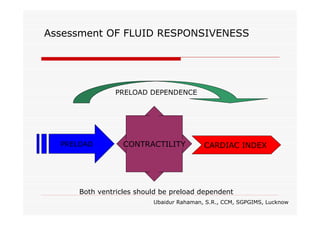
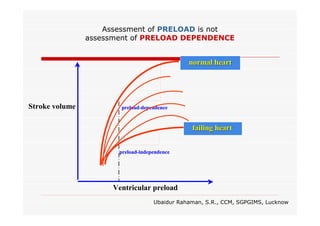
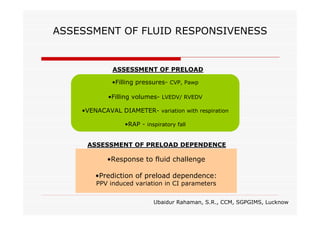
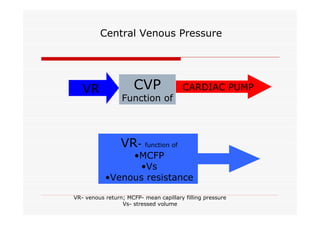
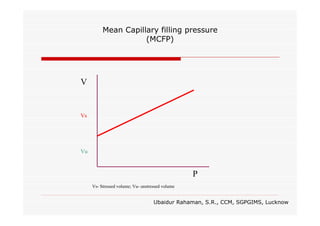
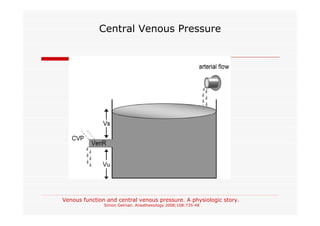
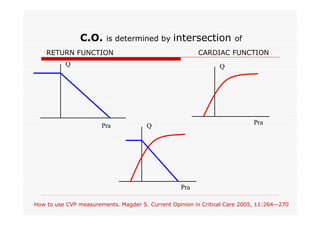
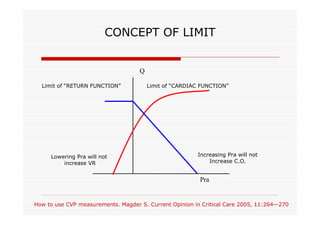
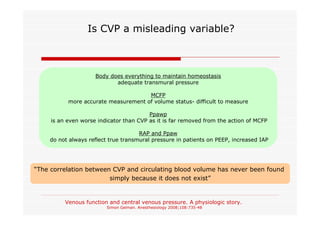
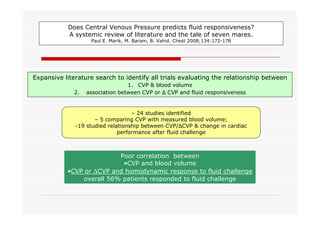
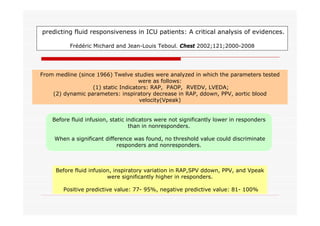
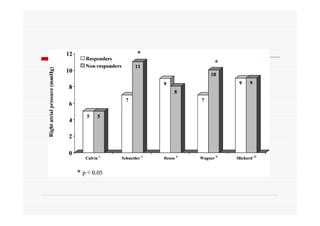
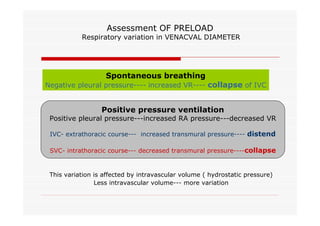
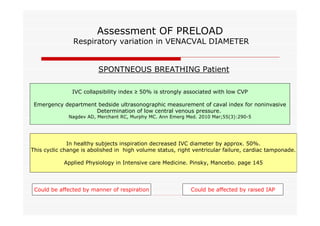
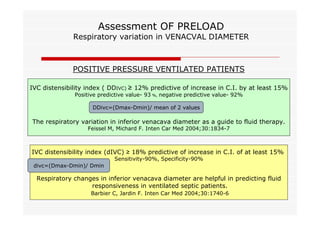
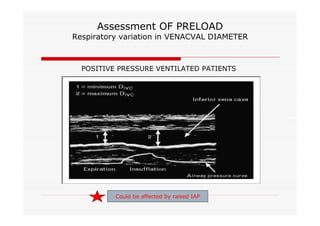
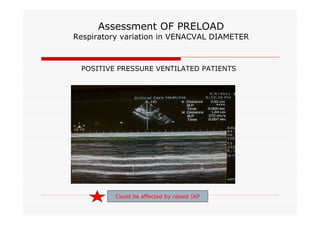
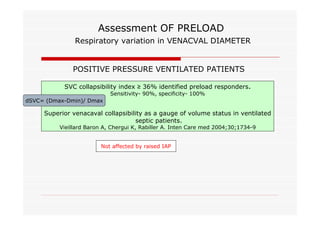
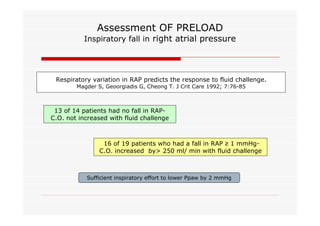
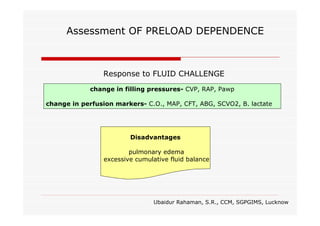
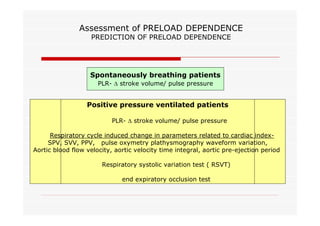
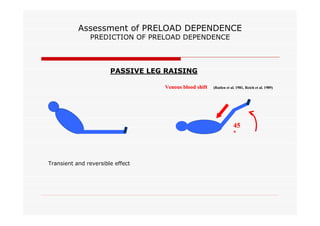
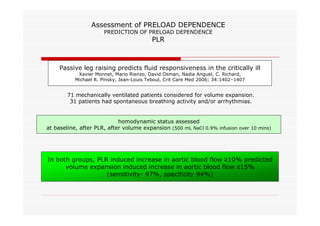
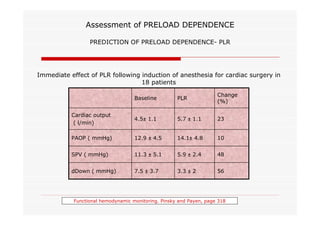
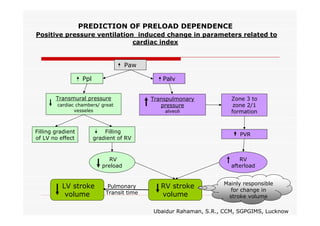
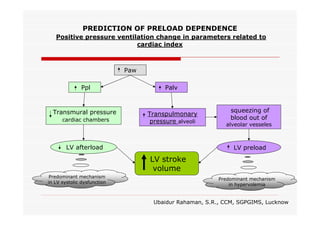
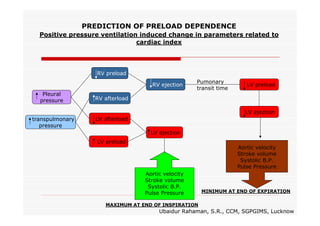
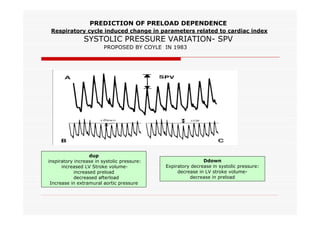
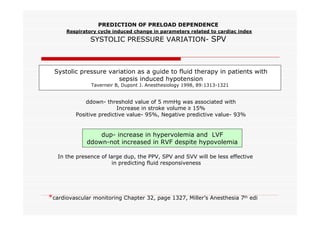
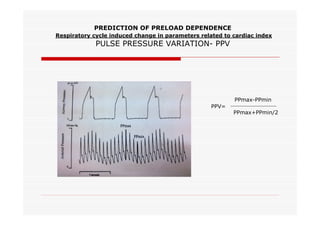
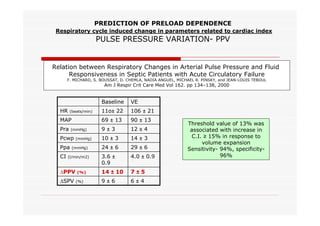
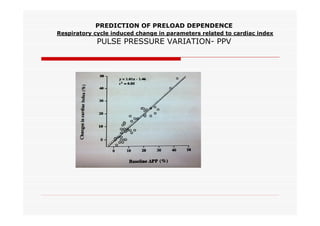
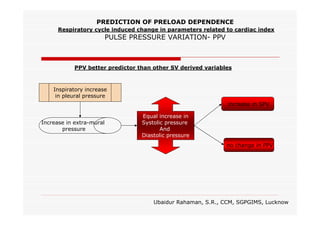
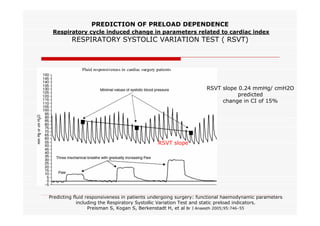
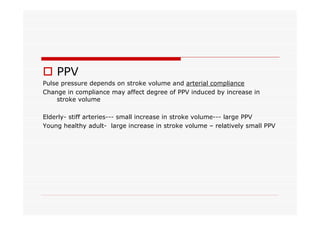
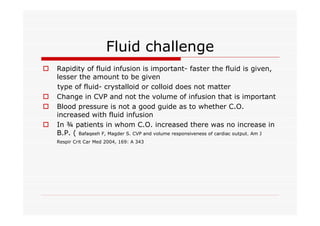
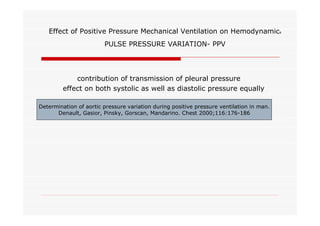
This document discusses fluid responsiveness in critically ill patients. It begins by defining fluid responsiveness as an increase in cardiac index after fluid infusion. It then describes three scenarios involving fluid resuscitation: patients with acute blood or fluid loss requiring immediate resuscitation, patients with suspected septic shock where early goal-directed therapy with fluids is important, and ICU patients who have already received fluids and their fluid responsiveness needs to be assessed. The document discusses various methods of assessing preload and preload dependence, including filling pressures, volumes, respiratory variations in inferior vena cava diameter, inspiratory drops in right atrial pressure, and predicting responsiveness through respiratory variations in parameters related to cardiac index. It emphasizes that preload alone