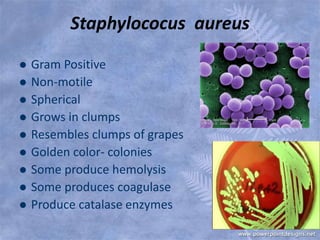
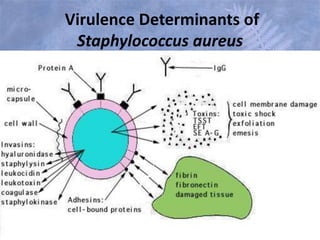
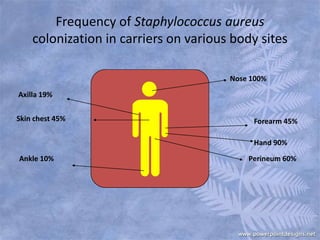
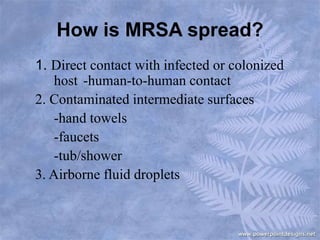
The document discusses the bacterium Staphylococcus aureus, including MRSA. It describes S. aureus's characteristics and how it can cause infections. MRSA was first identified in the 1940s when some S. aureus strains developed resistance to penicillin. It further discusses how MRSA is transmitted and the differences between CA-MRSA and HA-MRSA. Prevention, treatment options, and challenges like developing resistance are also covered at a high level.





































![Cont…
19. Duckworth G. Controlling methicillin-resistant Staphylococcus aureus. BMJ 2003;327: 1177–8[PMC free
article] [PubMed]
20. Voss A. Preventing the spread of MRSA. BMJ 2004;329: 521. [PMC free article] [PubMed]
21. Thompson DS. Methicillin-resistant Staphylococcus aureus in a general intensive care unit. J R Soc Med2004;97:
521–6 [PMC free article] [PubMed]
22. Rolinson GL, Stevens S, Batchelor FR, Cameron Wood J, Chain EB. Bacteriological studies on a new
penicillin. Lancet 1960;ii: 564–9 [PubMed]
23. Elek SD, Fleming PC. A new technique for the control of hospital cross infection. Lancet 1960;ii: 569–
72[PubMed]
24. Jevons MP. ‘Celbenin-resistant’ staphylococci. BMJ 1961;i: 124–5
25. Cox RA, Conquest C, Mallaghan C, Marples RR. A major outbreak of methicillin-resistant staphylococci caused by
a new phage type (EMRSA-16). J Hosp Infect 1995;29: 87–106 [PubMed]
26. Farrington M, Redpath C, Trundle C, Coomber S, Brown NM. Winning the battle, but losing the war: methicillin-
resistant Staphylococcus aureus (MRSA) at a teaching hospital. Q J Med 1998;91: 539–48[PubMed]
27. British Society for Antimicrobial Chemotherapy, Hospital Infection Society, Infection Control Nurses Association.
Revised guidelines for the control of methicillin-resistant Staphylococcus aureus infection in hospitals. J Hosp
Infect 1998;39: 253–90 [PubMed]
28. Emmerson AM, Enstone JE, Griffin M, Kelsey MC, Smyth ETM. The Second National Prevalence Survey of
Infection in Hospitals—overview of the results. J Hosp Infect 1996;32: 175–90 [PubMed]
29. Barrett SP, Mummery RV, Chattopadhyay. Trying to control MRSA causes more problems than it solves. J Hosp
Infect 1998;39: 85–93 [PubMed]
30. Farrington M, Redpath C, Trundle C, Brown NM. Controlling MRSA. J Hosp Infect 1999;40: 251–4[PubMed]
•](https://image.slidesharecdn.com/presentation1-150131122641-conversion-gate01/85/MRSA-44-320.jpg)
![Cont…
31. Cooper BS, Stone SP, Kibbler CC, et al. Isolation measures in the hospital management of methicillin-
resistant Staphylococcus aureus (MRSA): systematic review of the literature. BMJ 2004;329: 533–9[PMC free
article] [PubMed]
32. Wertheim HFK, Vos MC, Boelens HAM, et al. Low prevalence of methicillin-resistant Staphylococcus
aureus (MRSA) at hospital admission in the Netherlands: the value of the search and destroy and restrictive
antibiotic use. J Hosp Infect 2004;56: 321–5 [PubMed]
33. Marshall C, Wolfe R, Kossman T, Wesselingh S, Harrington G, Spelman D. Risk factors for acquisition of
methicillin-resistant Staphylococcus aureus by trauma patients in the intensive care unit. J Hosp Infect2004;57:
245–52 [PubMed]
34. Silvestri L, van Saene HKF, Milanese M, et al. Prevention of MRSA pneumonia by oral vancomycin
decontamination: a randomised trial. Eur Respir J 2004;23: 921–6 [PubMed]
35. de la Cal MA, Cerda E, van Saene HKF, et al. Effectiveness and safety of enteral vancomycin to control
endemicity of methicillin-resistant Staphylococcus aureus in a medical/surgical intensive care unit. J Hosp
Infect 2004;56: 175–83 [PubMed]
36. Van Saene HKF, Weir WI, de la Cal MA, Silvestri L, Petros AJ, Barrett SP. MRSA—time for a more pragmatic
approach. J Hosp Infect 1998;56: 175–83
37. Howe R, Monk A, Wootton M, Wash T, Enright MC. Vancomycin susceptibility within methicillin-
resistant Staphylococcus aureus lineages. Emerg Infect Dis 2004;10: 855–7 [PMC free article] [PubMed]
38. Dryden MS, Dailly S, Crouch M. A randomised, controlled trial of tea tree topical preparations versus a standard
topical regime for the clearance of MRSA colonisation. J Hosp Infect 2004;56: 283–6 [PubMed]
39. Pancheco-Fowler V, Gaonakar T, Wyer PC, Modak K. Antiseptic impregnated endotracheal tubes for the
prevention of bacterial colonisation. J Hosp Infect 2004;57: 170–4 [PubMed]
40. French GL, Otter J, Shannon KP, Adams NMT, Watling D, Parks MJ. Tackling hospital environmental
contamination with methicillin-resistant Staphylococcus aureus (MRSA): a comparison between conventional
terminal cleaning and hydrogen peroxide vapour decontamination. J Hosp Infect (in press)[PubMed]](https://image.slidesharecdn.com/presentation1-150131122641-conversion-gate01/85/MRSA-45-320.jpg)
