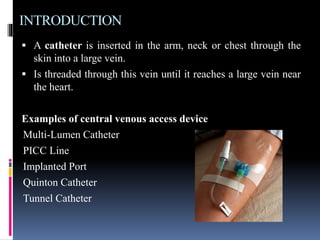
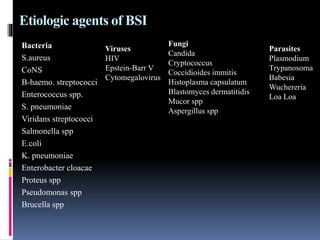
Central line-associated bloodstream infections (CLABSI) occur when microbes enter the bloodstream via central venous access devices, which can lead to serious health complications and are largely preventable. Risk factors include age extremes, malnutrition, immunosuppressive therapies, and prolonged hospital stays, while bacteria are the most common etiological agents. Diagnosis involves blood culture, with prevention strategies essential in reducing incidence and improving patient outcomes.