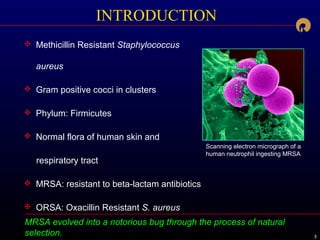
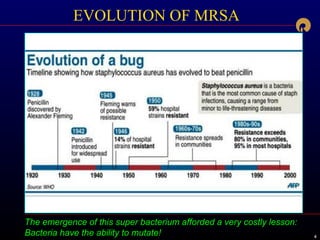
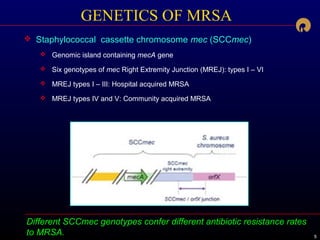
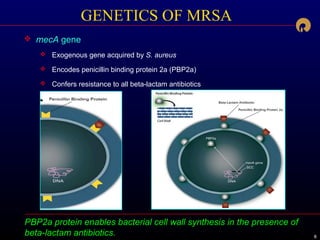
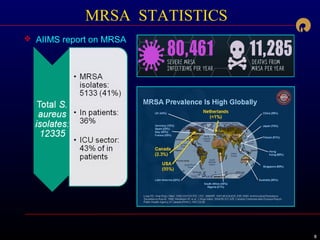
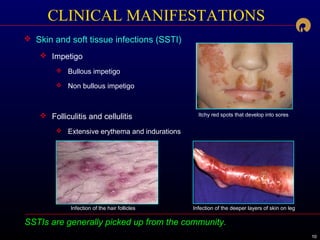
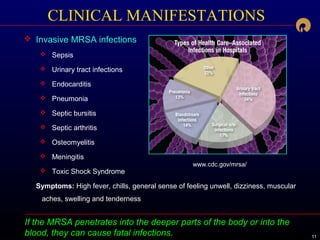
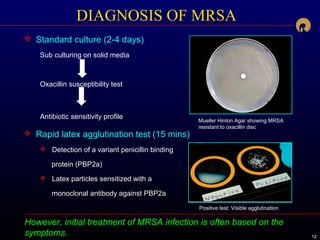
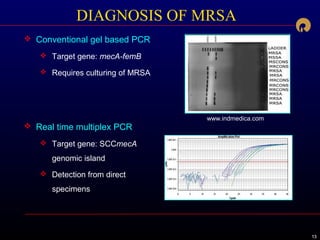
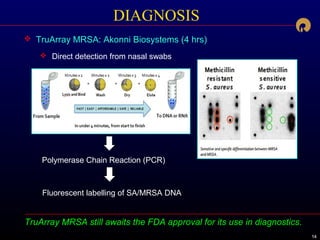
This document summarizes information about methicillin-resistant Staphylococcus aureus (MRSA), including its evolution, genetics, transmission, clinical manifestations, diagnosis, treatment, ongoing research, and prevention. MRSA evolved through natural selection to become resistant to beta-lactam antibiotics. It carries a genetic element called SCCmec that confers this resistance. MRSA can cause a range of infections through skin-to-skin contact and spread in both healthcare and community settings. Diagnosis involves culture and identification of the mecA gene which encodes resistance. Treatment depends on the site and severity of infection, utilizing antibiotics like vancomycin or decolonization regimens. Ongoing research explores new drug combinations