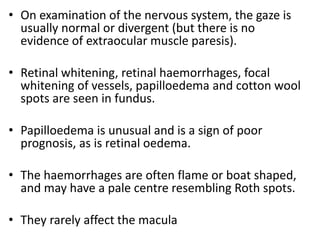
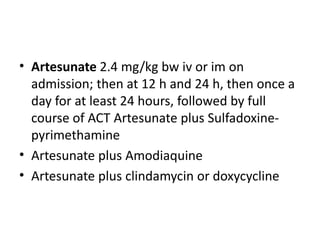
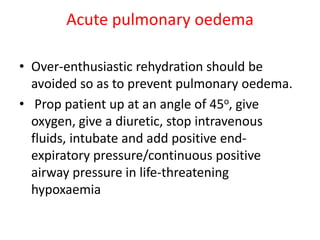
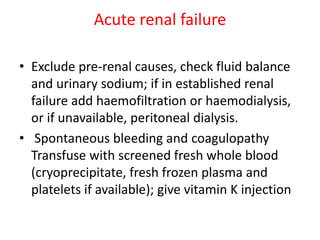
Malaria is a protozoan infection transmitted by mosquitoes that infects red blood cells. P. falciparum malaria can cause severe complications such as cerebral malaria, acute renal failure, pulmonary edema, liver dysfunction, hypoglycemia, and acidosis due to parasite sequestration in vital organs. Treatment involves antimalarial drugs like artesunate or quinine plus supportive care for organ dysfunction. Cerebral malaria requires airway control, anticonvulsants, treatment of hypoglycemia, and blood transfusion for severe anemia.





































![• Quinine 20 mg salt/kg bw on admission (iv
infusion over 4 hrs, then 10 mg/kg bw every 8
h; infusion rate should not exceed 5 mg
salt/kg bw per hour; course for 3 days. 7 days
for malaria acquired in SE Asia[4] Doxycyclined
100mgs BID for 7 days OR Clindamycin 20mg
base/kg/day divided in three doses for 7
days[4] in pregnancy.](https://image.slidesharecdn.com/malariapart1-151018194308-lva1-app6892/85/Malaria-part-1-58-320.jpg)