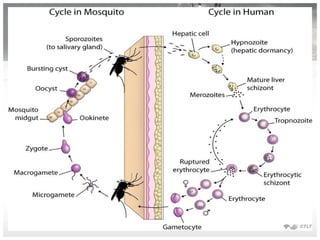
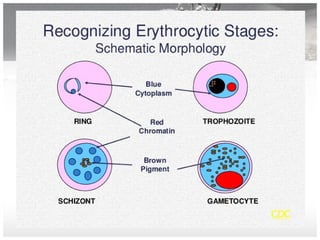
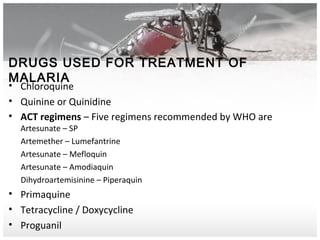
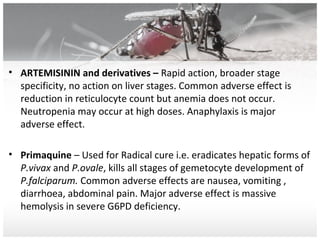
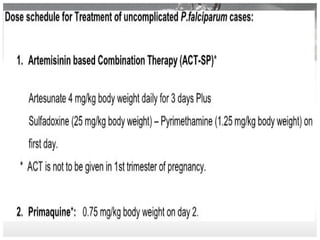
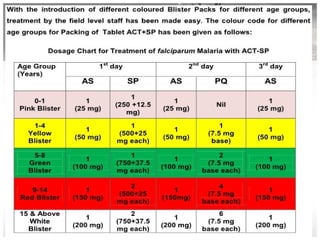
The document discusses malaria, caused by parasites of the Plasmodium genus transmitted via mosquito bites. It affects over 100 countries and kills approximately 2,000 people per day. The most common species causing malaria in India are P. vivax, P. falciparum, P. ovale, and P. knowlesi, with P. falciparum being the most lethal. Malaria symptoms include fever, fatigue, nausea, and in severe cases can include cerebral malaria, acidosis, anemia, renal failure, pulmonary edema, hypoglycemia, and death. Diagnosis involves examining blood smears under a microscope for parasites. Treatment depends on the Plasmodium species and may include chloroquine,