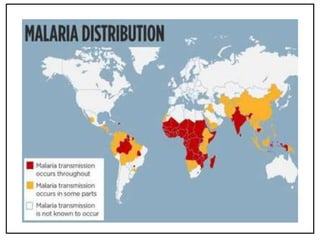
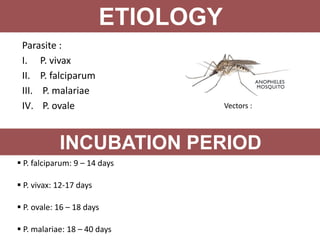
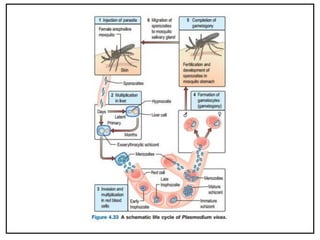
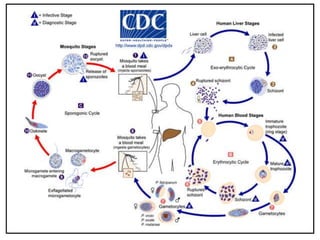
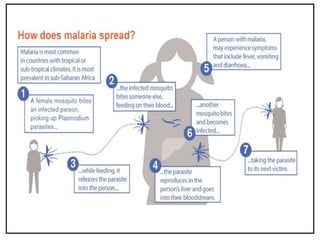
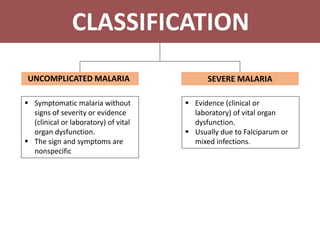
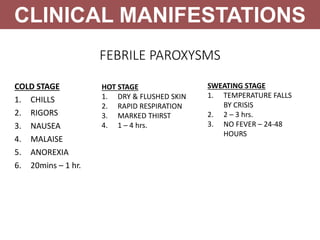
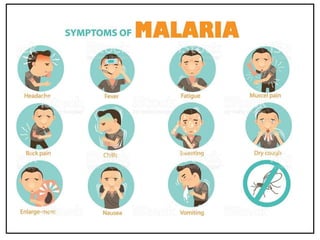
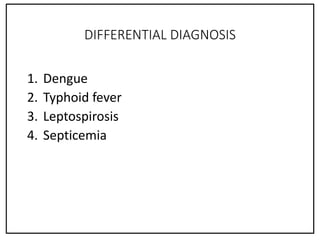
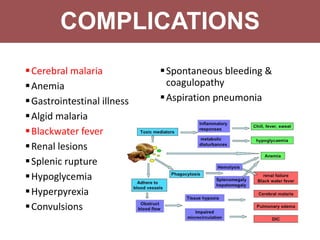
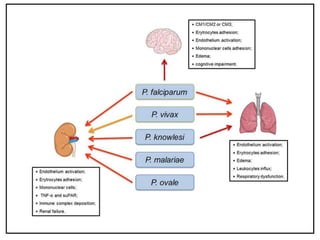
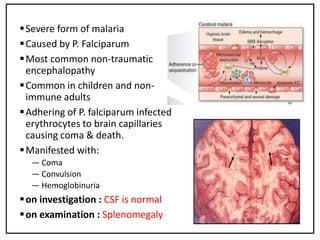
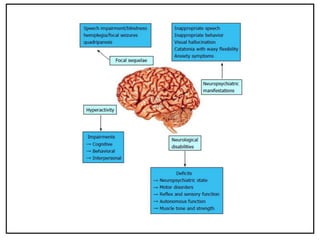
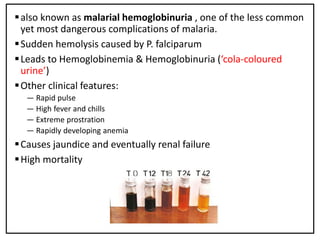
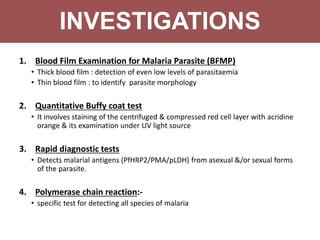
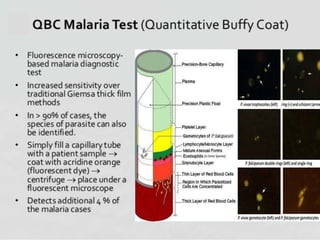
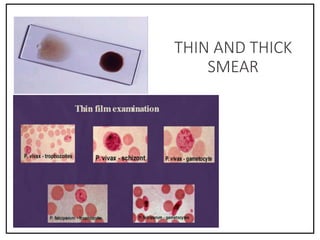
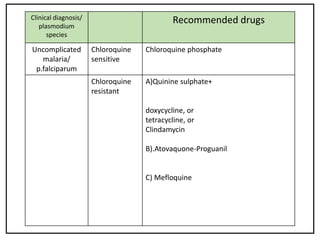
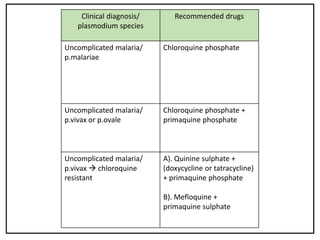
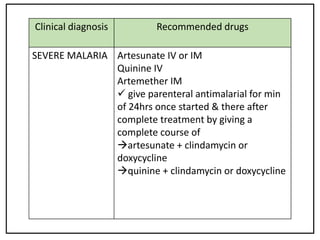
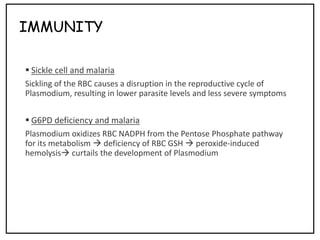
The document summarizes information about malaria, including that it is caused by parasites transmitted via mosquito bites, with 350-500 million cases annually. It discusses the four Plasmodium species that cause malaria and their incubation periods. Malaria symptoms include febrile paroxysms with chills, fever, and sweating stages. Complications include cerebral malaria, anemia, and blackwater fever. Diagnosis involves blood film examination, and treatment depends on parasite species and disease severity, usually requiring around two weeks.