This document provides an overview of malaria, including:
1. The five Plasmodium species that cause human malaria, with P. falciparum and P. vivax present in Sri Lanka.
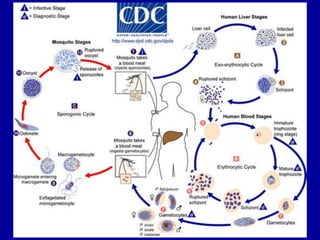
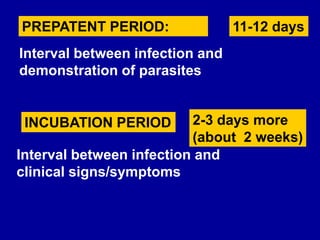
2. The life cycles of the parasites, including their prepatent and incubation periods in the human host.
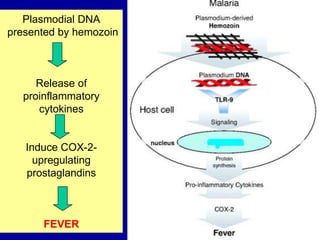
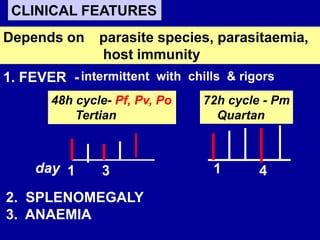
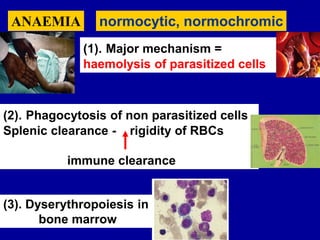
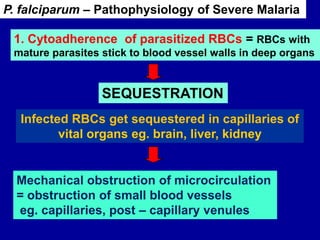
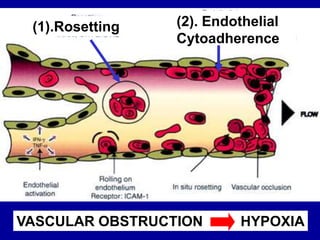
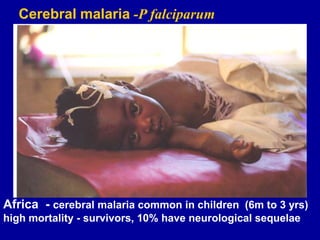
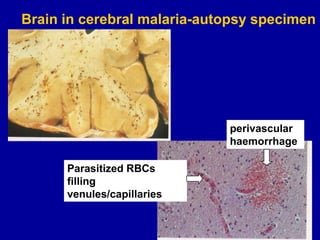
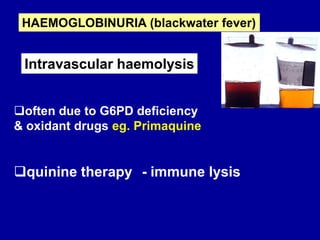
3. The pathophysiology of malaria, including the erythrocytic cycle causing haemolysis, host immune response, and mechanisms of severe malaria like cytoadherence.
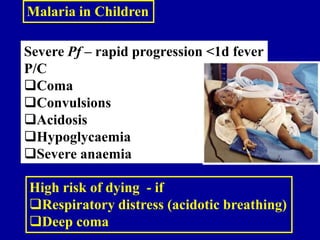
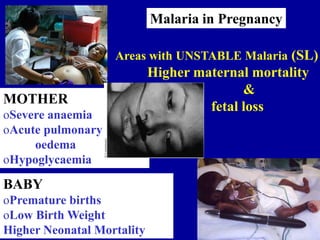
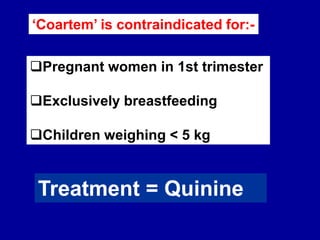
4. Clinical features ranging from uncomplicated to severe malaria, and differences between recrudescence and relapse.











![Interfere with microcirculation
1. Tissue hypoxia
2. Nitric oxide [NO] release
2. Rosetting = Parasitized RBCs stick to
uninfected RBCs
P. falciparum – Pathophysiology of Severe Malaria
3. Rigid parasitized RBCs get stuck in narrowed
capillary lumen](https://image.slidesharecdn.com/malaria-clinical-130612042427-phpapp02/85/Malaria-clinical-20-320.jpg)


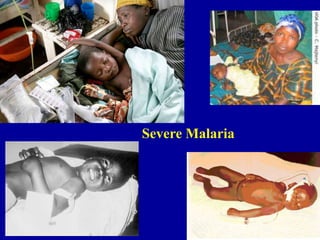
![Severe Malaria
• Impaired level of
consciousness, COMA
• Convulsions
• Generalized and
localized
neurological signs
Cerebral
Pathogenesis Clinical Features
Renal
• Acute tubular necrosis -
sluggish blood flow and hypotension.
•Intravascular haemolysis
•Oliguria
• Haemoglobinuria
• Acute Renal Failure [ARF]
Sluggish flow caused by
sticky knobs on parasitized
redcells leading to stagnant
hypoxia and vascular damage.](https://image.slidesharecdn.com/malaria-clinical-130612042427-phpapp02/85/Malaria-clinical-24-320.jpg)
![Severe Malaria: Common Clinical Manifestations 2
Pathogenesis Clinical Features
Increased pulmonary
capillary permeability
• Cough
• Pulmonary oedema
[ARDS]
•Bronchopneumonia
•Elevated serum enzyme levels
•Prolonged prothrombin time
Jaundice
(mainly haemolytic)
Bleeding
Respiratory
Hepatic](https://image.slidesharecdn.com/malaria-clinical-130612042427-phpapp02/85/Malaria-clinical-25-320.jpg)
![Severe Malaria: Common Clinical Manifestations 3
BLOOD Severe anaemia – Hb < 5g/dl
Hypoglycaemia
Acidaemia
Shock
Disseminated Intravascular Circulation [DIC]
Multiple Organ Dysfunction [MODS]](https://image.slidesharecdn.com/malaria-clinical-130612042427-phpapp02/85/Malaria-clinical-26-320.jpg)
![1. Impairment of consciousness
Glasgow Coma Scale [adults] & Blantyre Scale [children]
2. Prostration – inability to sit unassisted in a child.
In infant not old enough to sit, inability to feed
[on examination - not just told in history]
3. Hyperparasitaemia >4% in non-immune [SL]
SEVERE MALARIA – 2000 WHO
Treat any patient as SEVERE MALARIA
if physician is worried about Signs & Symptoms
BUT](https://image.slidesharecdn.com/malaria-clinical-130612042427-phpapp02/85/Malaria-clinical-27-320.jpg)





![MALARIA ENDEMICITY
STABLE OR UNSTABLE TRANSMISSION
Hyper/holo endemic
High anopheline biting
frequency
Severe malaria in
6 months -3 yrs age
Older – asymptomatic
parasitaemic
[PREMUNITION]
Pregnancy – severe
malaria
Spleen rate .50% in
children 2-9yrs
UNSTABLE MALARIA
[Sri Lanka,Thailand, Cambodia]
Meso / hypoendemic
Severe malaria in all ages
Cerebral malaria > common
Spleen rate in children
<50%
STABLE MALARIA
[AFRICA]](https://image.slidesharecdn.com/malaria-clinical-130612042427-phpapp02/85/Malaria-clinical-39-320.jpg)




![44
ANTIGEN DETECTION
RAPID DIAGNOSTIC TESTS [RDTs]
Dipstick/card methods
1. Most useful commercial tests detecting
BOTH Pf + Pv
Detects
parasite Lactate dehydrogenase ( pLDH)
depends on LIVE parasites
CAN USE TO TEST DRUG RESISTANCE](https://image.slidesharecdn.com/malaria-clinical-130612042427-phpapp02/85/Malaria-clinical-44-320.jpg)
![2. RDTs – sensitivity is low
(won’t detect below 100 – 200 parasites/μl)
45
ANTIGEN DETECTION
RAPID DIAGNOSTIC TESTS [RDTs]
WHO malaria RDT performance evaluation - Round 2
1. High cost
Disadvantages
Advantages
1. Easy to do in field
2. Don’t need trained persons](https://image.slidesharecdn.com/malaria-clinical-130612042427-phpapp02/85/Malaria-clinical-45-320.jpg)


![Malaria Treatment in Sri Lanka
Vivax malaria
1. Chloroquine –
blood schizonticide
2. Primaquine – Kills
hypnozoites &
gametocytes
Falciparum Malaria
Combination therapy to limit
Development of drug resisitance
CO-ARTEMETHER
[Artemether & Lumefantrine]
& Primaquine
Severe Pf – Quinine](https://image.slidesharecdn.com/malaria-clinical-130612042427-phpapp02/85/Malaria-clinical-48-320.jpg)


![Assessment of Therapeutic
Response to Anti-malarials
(1) Parasite Clearance Time (PCT)
Time between beginning the anti-malarial
treatment and the first –ve blood film
(2) Fever Clearance Time (FCT)
Time from beginning anti- malarial treatment
until the patient is apyrexial [no fever]](https://image.slidesharecdn.com/malaria-clinical-130612042427-phpapp02/85/Malaria-clinical-52-320.jpg)








