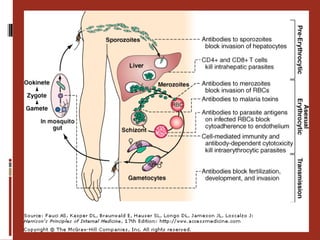
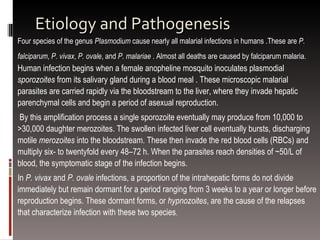
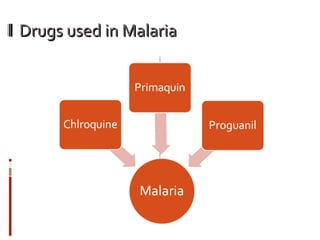
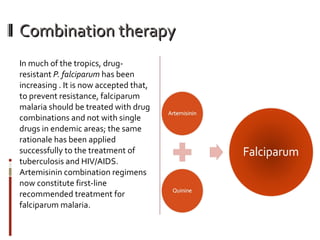
Malaria is a protozoan disease transmitted through mosquito bites that infects over 3 billion people and causes over 1 million deaths annually. It is caused by Plasmodium parasites, notably P. falciparum which is responsible for most deaths. The parasites infect the liver and then red blood cells, multiplying and causing symptoms like fevers and in severe cases, complications affecting vital organs. Treatment of malaria varies by parasite species but increasingly involves artemisinin combination therapy to prevent drug resistance from developing.