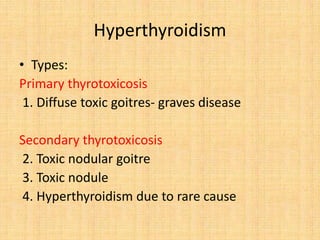
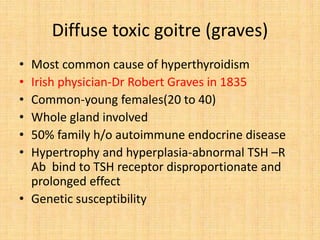
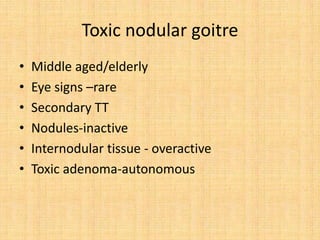
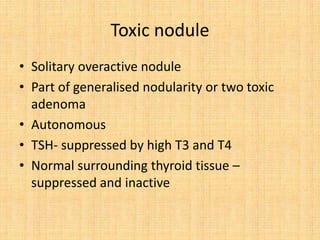
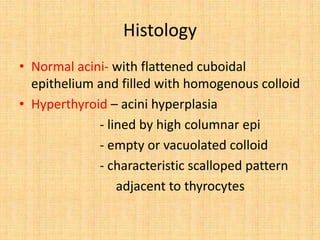
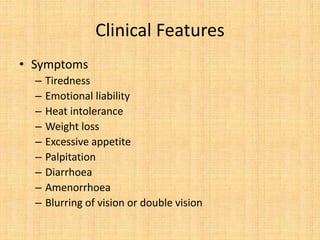
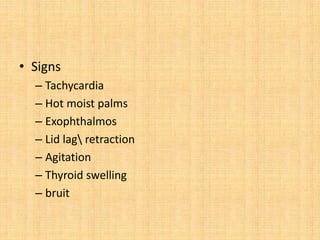
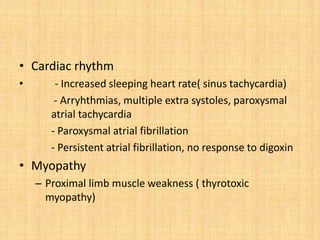
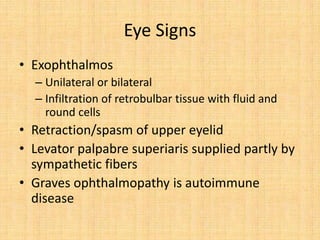
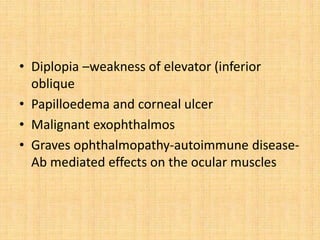
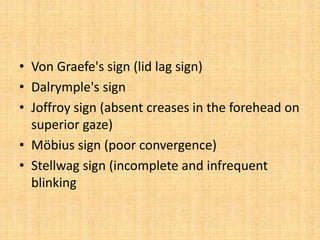
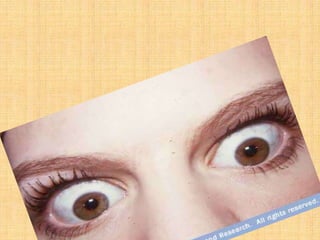
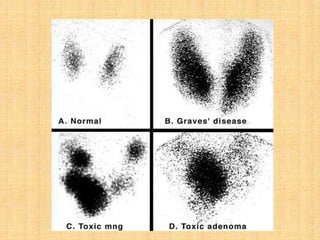
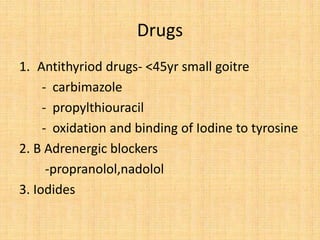
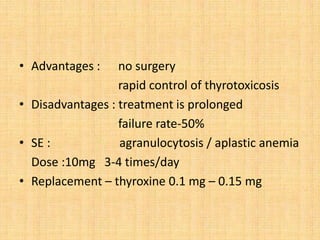
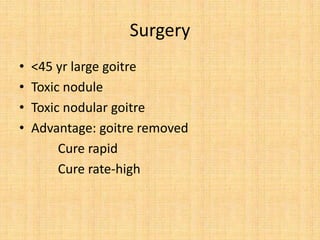
Hyperthyroidism is a hypermetabolic state caused by increased thyroid secretion. There are several types, including Graves' disease (the most common cause), toxic nodular goitre, and toxic adenoma. Clinical features include symptoms like fatigue, heat intolerance, and weight loss, as well as signs like tachycardia, eye changes, and thyroid swelling. Diagnosis involves clinical evaluation, thyroid function tests, and scans. Treatment options are antithyroid drugs, surgery, and radioactive iodine.