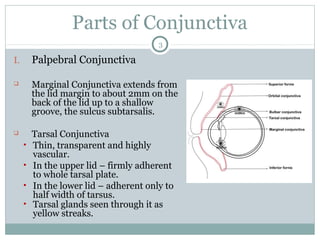
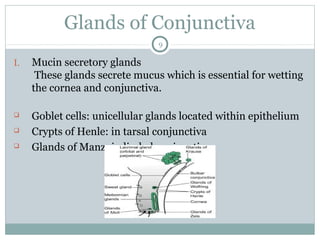
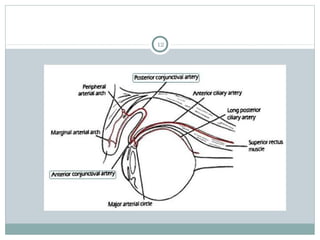
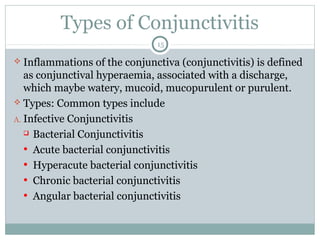
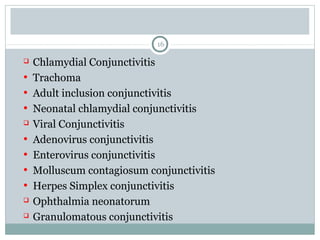
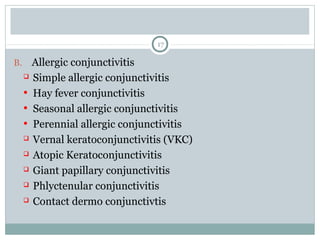
This document provides an overview of the anatomy of the conjunctiva and classification of conjunctivitis. It describes the parts and structure of the conjunctiva, including its epithelium, adenoid and fibrous layers. It also details the glands, blood supply, nerves and types of conjunctivitis. The conjunctiva has palpebral, bulbar, and forniceal regions and contains goblet cells, glands of Krause and glands of Wolfring. Conjunctivitis can be infective from bacteria, viruses, or chlamydia. It can also be allergic, cicatricial, or toxic in nature.