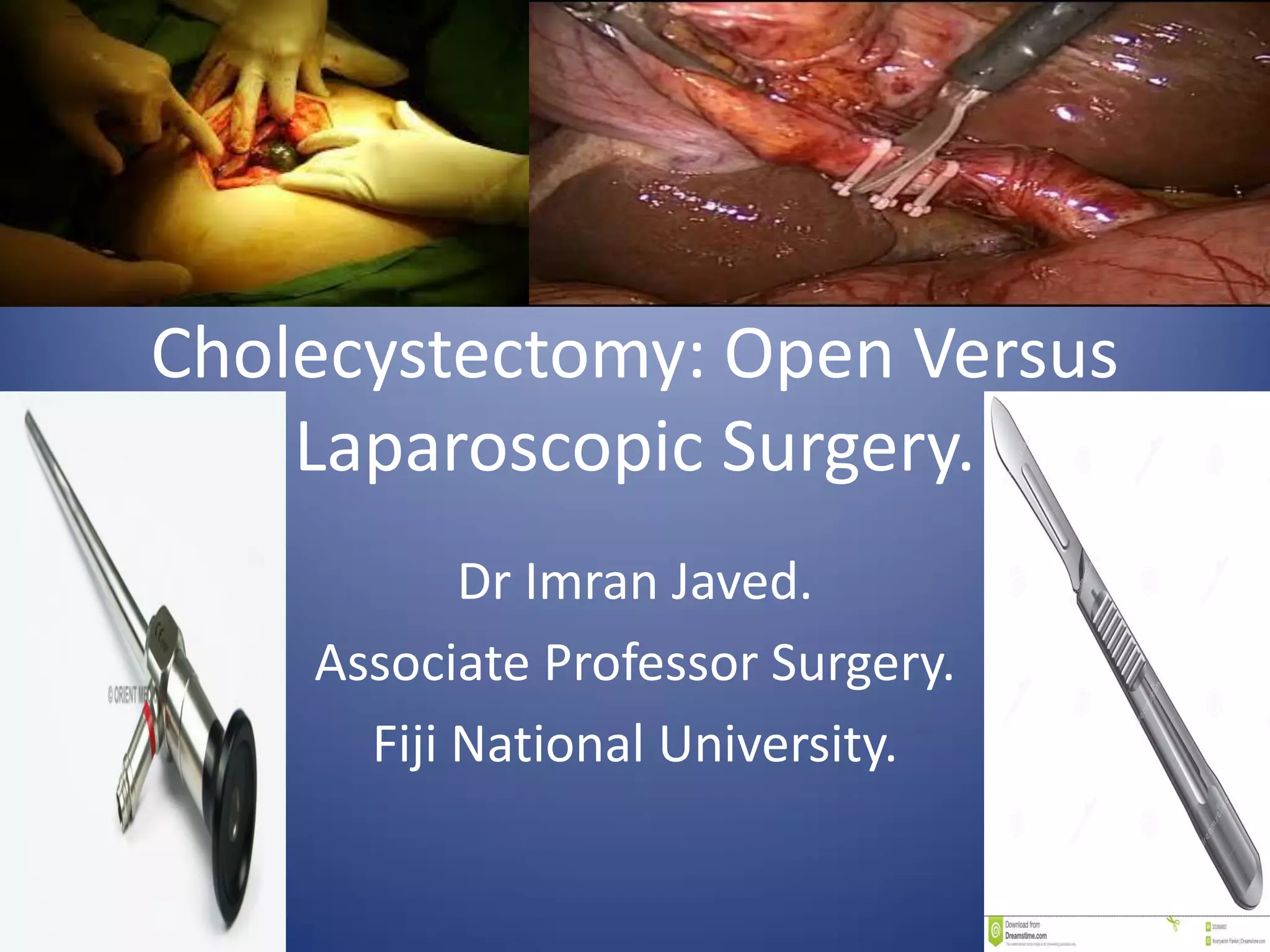
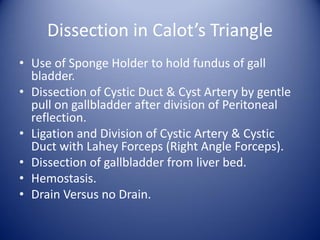
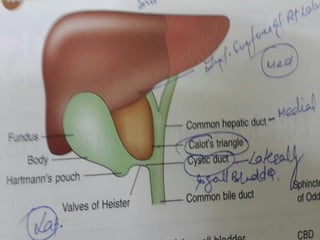
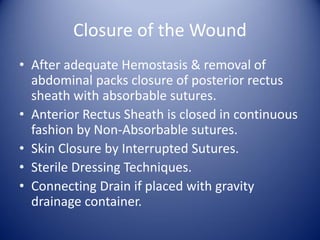
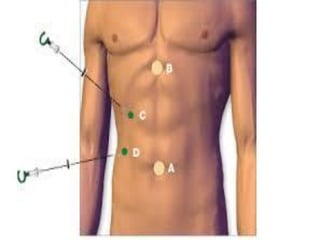
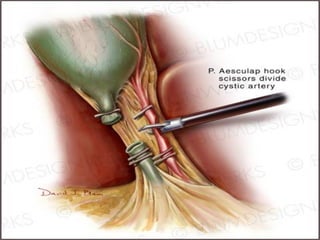
This document compares open and laparoscopic cholecystectomy procedures. Open cholecystectomy is easier to perform and more cost effective, but results in a longer hospital stay and poorer cosmetic outcomes. Laparoscopic cholecystectomy is now the gold standard, providing shorter recovery time and fewer complications, but requires specialized equipment and training and carries a higher risk of duct injuries. Both approaches are appropriate depending on the patient's condition and surgeon's expertise.