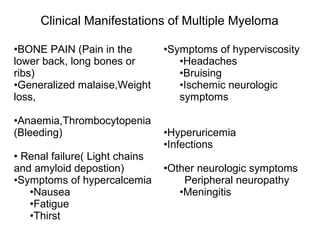
Multiple myeloma is a cancer of plasma cells that results in overproduction of abnormal antibodies in the bone marrow. It commonly causes bone pain, fractures, anemia, and kidney problems. Risk factors include age over 60 and exposure to chemicals like pesticides, radiation, or certain industrial chemicals. Treatment may include chemotherapy, steroids, stem cell transplantation, radiation, surgery, and newer drugs like thalidomide, lenalidomide, and bortezomib to improve outcomes. Despite recent advances, multiple myeloma remains incurable and patients often relapse, highlighting the need for additional therapeutic options.