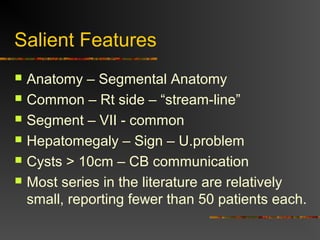
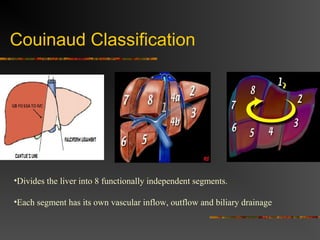
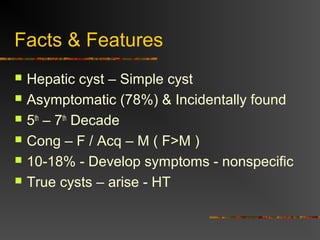
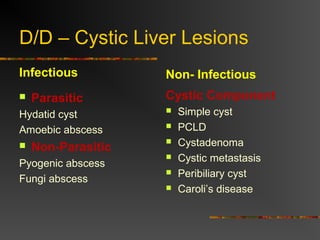
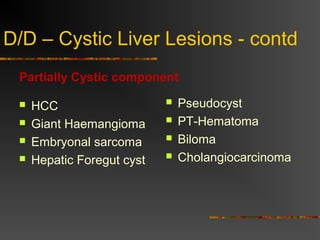
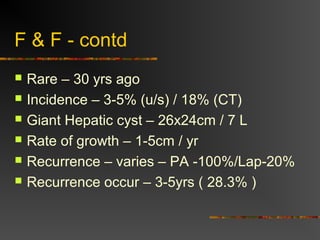
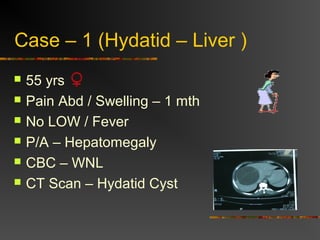
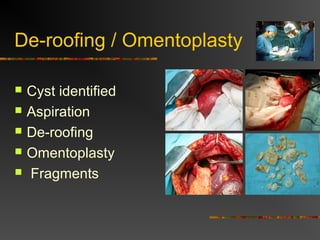
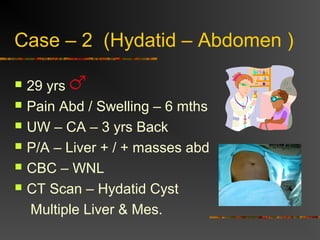
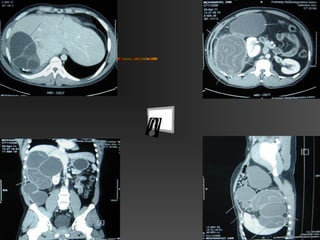
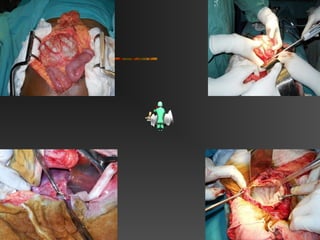
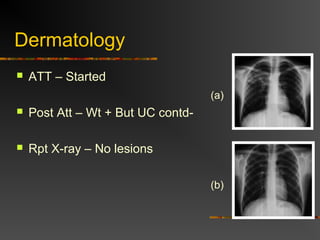
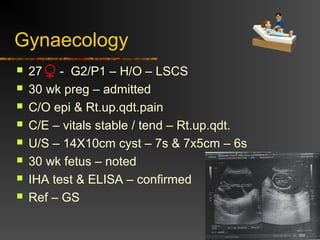
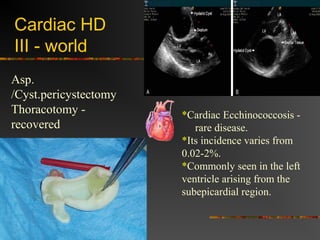
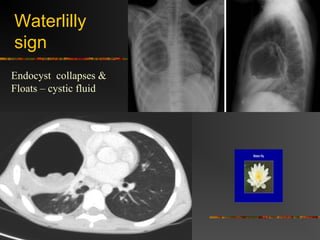
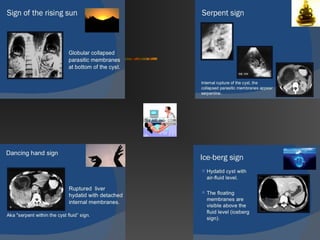
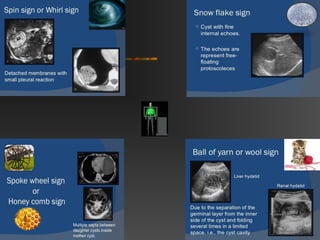
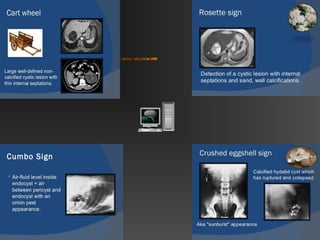
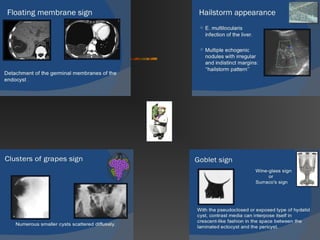
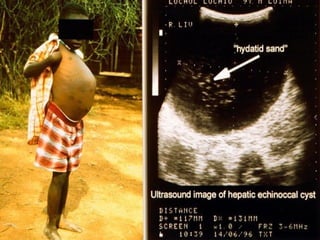
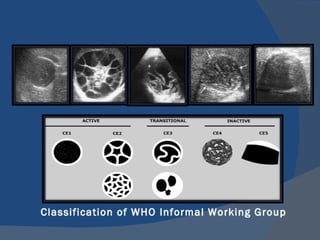
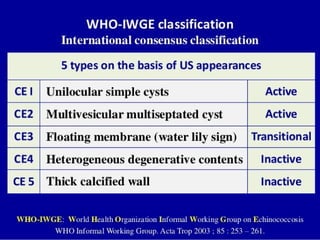
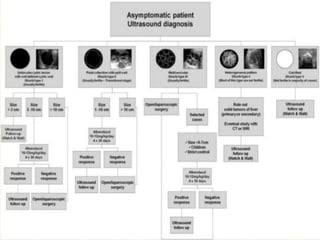
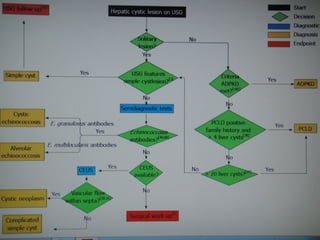
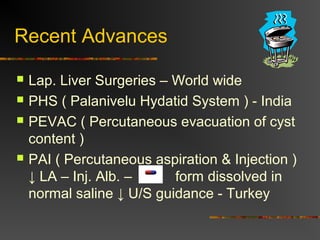
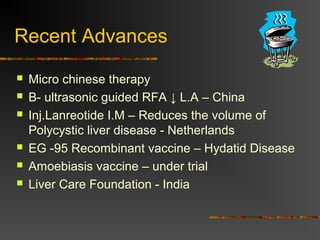
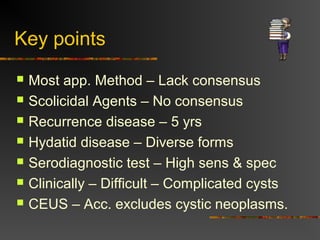
The document provides an in-depth discussion on liver cysts, including their classification, types, and personal case studies dealing with hydatid cysts. It covers salient features, complications, and recent advances in treatment options while emphasizing the need for standardized approaches. Key points highlighted include the challenges in diagnosis and management as well as the incidence of various types of cysts across different specialties.