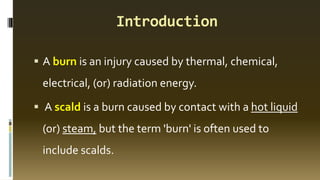
This topic is very important for MBBS Students as for sure it will be reflecting upon in the theoretical as well as clinical aspect. They should be familiar with the clinical findings of a burn patient, to differentiate among them the stages of burns as well as to calculate the fluid requirements accordingly. This topic covers above all aspects of burns.....



![Classification of Burns
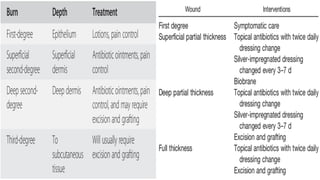
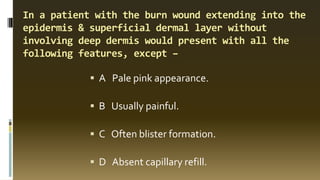
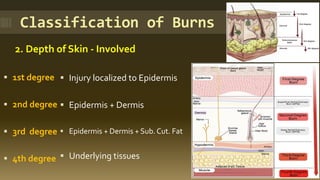
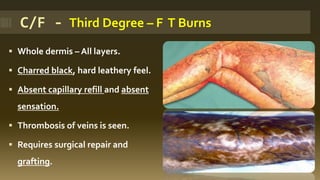
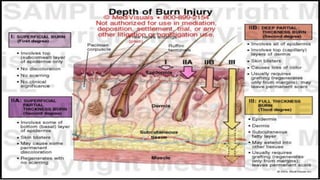
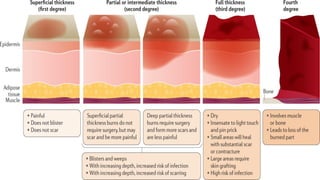
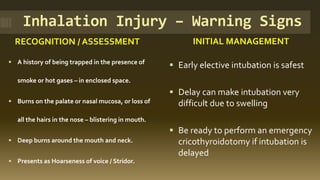
3.Thickness of Skin - Involved
▪ Superficial
▪ Partial thickness
[SP / DP]
▪ Full thickness
▪ 1st degree
▪ 2nd degree
▪ 2nd degree
▪ 3rd degree](https://image.slidesharecdn.com/burns-251009070438-bd20b18a/85/Burns-Types-Clinical-Features-Management-7-320.jpg)



![Burn zones [Jackson’s]](https://image.slidesharecdn.com/burns-251009070438-bd20b18a/85/Burns-Types-Clinical-Features-Management-16-320.jpg)
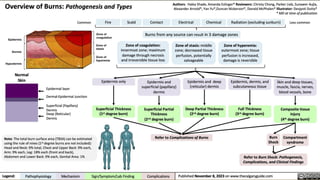


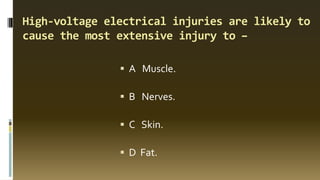
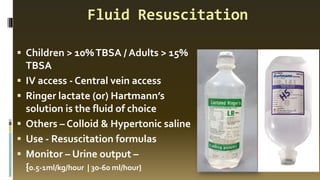
![Burn causes – Likely depth
Cause of burn Probable depth of burn
Scald Superficial – Can be deep
Flash Burns Deep Dermal to FT
Flame Burns Mixed deep dermal + Full thickness
Alkali Burns Deep dermal [or] Full thickness
Acid Burns Weak – Superficial / Strong – Deep dermal
Electric Burns Full thickness](https://image.slidesharecdn.com/burns-251009070438-bd20b18a/85/Burns-Types-Clinical-Features-Management-27-320.jpg)
![Immediate [Pre-hospital Care]
▪ Remove from source of injury
▪ Clothing to be removed
▪ Cool the burn wound – 10 - 20mts –
no cold H2o
▪ Check for other injury
▪ Cleaning & Chemoprophylaxis
▪ Ensure rescuer safety](https://image.slidesharecdn.com/burns-251009070438-bd20b18a/85/Burns-Types-Clinical-Features-Management-32-320.jpg)


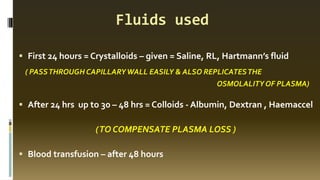
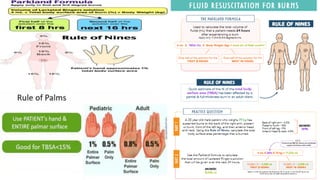
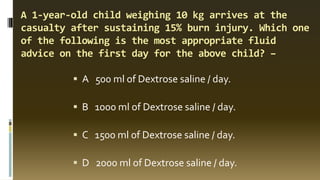
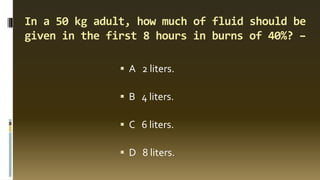
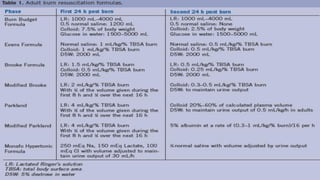
![Parkland Formula – Commonly used
▪ 4ml x % burn x weight (kg) = volume [ml] - 24 hours
▪ Max. % considered = 50%
▪ First 8 hours ½ of vol. – Rest in next 16 hours = 24 hours
▪ Next 24 hours = ½ of first day fluids](https://image.slidesharecdn.com/burns-251009070438-bd20b18a/85/Burns-Types-Clinical-Features-Management-37-320.jpg)