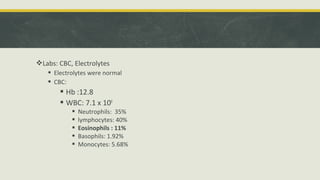
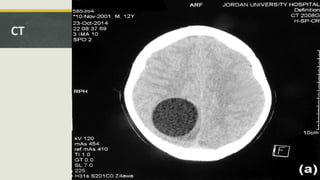
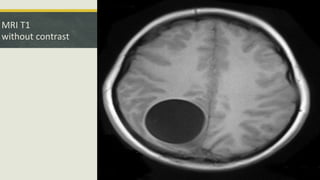
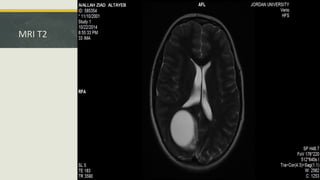
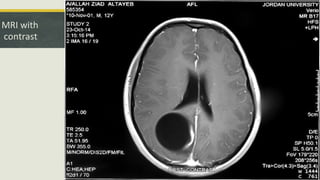
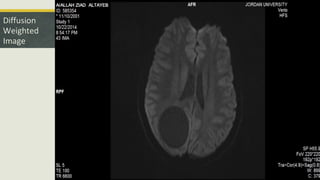
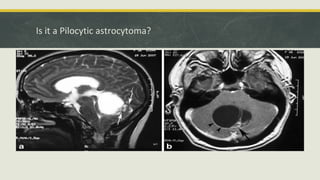
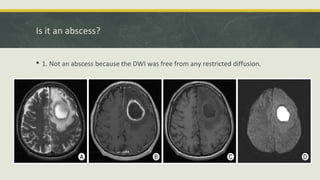
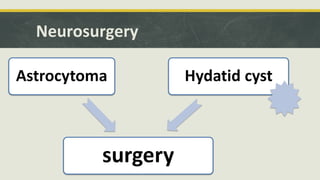
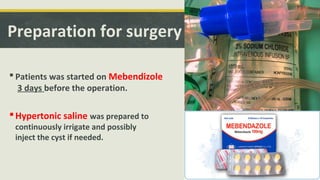
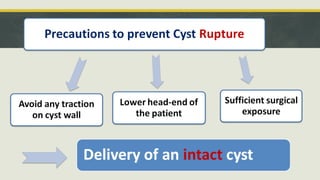
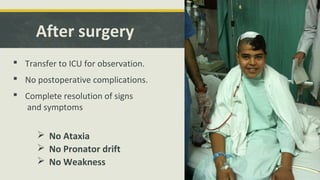
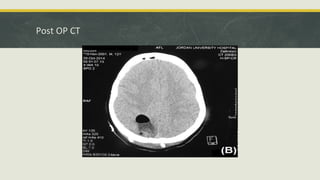
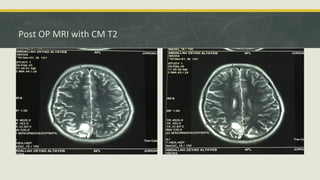
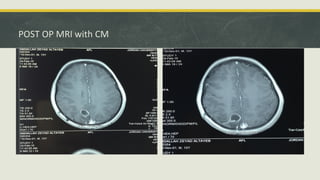
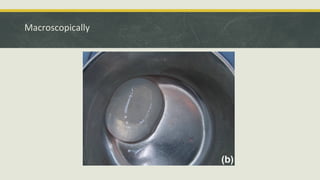
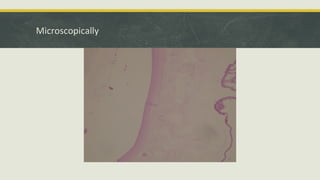
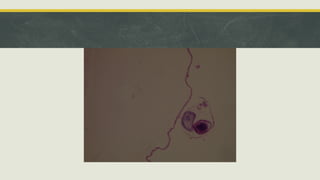
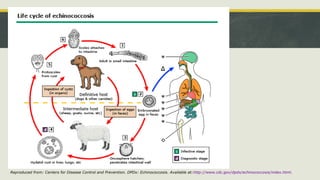
This document describes the case of a 13-year-old boy who presented with a one month history of progressive headaches, left-sided weakness, and mild bilateral papilledema. Imaging revealed a cystic lesion in the right parieto-occipital region. The patient underwent a neurosurgical procedure to remove the intact cyst, which was confirmed to be an isolated intracranial hydatid cyst based on pathology. Hydatid cysts are caused by the tapeworm Echinococcus and most commonly involve the liver and lungs. Intracranial involvement is rare but can cause signs of increased intracranial pressure like this case.