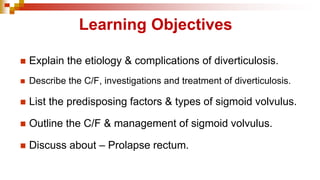
This PPT covers 3 interesting topics - Diverticulosis, Volvulus & Rectal Prolapse. All 3 topics are important for MBBS Students - for both theoretical purpose & clinical purpose. Even though they are rare diseases of the colon, questions related to this topic are commonly being asked in most of the competitive exams....


![D Disease - Introduction
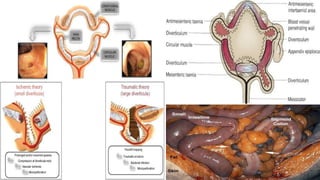
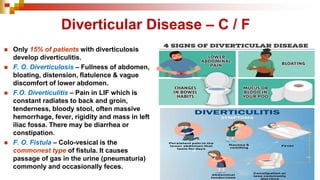
◼ They are {Diverticula} herniations of colonic mucosa
through circular muscles at the points where blood
vessels penetrate the bowel wall.
◼ It is more commonly localized to sigmoid colon (70-
90%) but can affect the whole colon. [Rectum is not
affected].
◼ It is rare in Asian & African countries because of the
high fiber diet. It is common in western countries.
◼ The combination of altered collagen structure with
ageing, disordered motility and increased
intraluminal pressure, is seen most notably in the
narrow sigmoid colon. Whereas the rectum has a
complete muscular coat and a wider lumen and is
thus very rarely affected.](https://image.slidesharecdn.com/diverticulosisvolvulusrectalprolapse-250727032604-5de6cd6f/85/Diverticulosis-Volvulus-Rectal-prolapse-pdf-4-320.jpg)



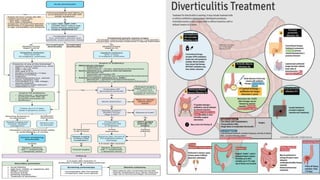
![Diverticular Disease – Treatment
Medical
[Acute]
• Bowel rest
• Antibiotics
• Antispasmodics
• High fiber diet
• Bulk purgatives
• Avoid
constipation
Surgical
[Indications]
• Peritonitis
• FOM treatment
• R. Diverticulitis
• Abscess –can be
drained – PC by
CT-guidance](https://image.slidesharecdn.com/diverticulosisvolvulusrectalprolapse-250727032604-5de6cd6f/85/Diverticulosis-Volvulus-Rectal-prolapse-pdf-14-320.jpg)



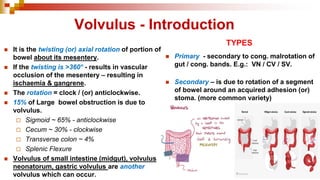
![Sigmoid Volvulus – Treatment
◼ Decompression:
- Sigmoidoscope (or) flatus tube inserted into
rectum / pt. passes flatus & faeces --> successful.
◼ If de-rotation does not occur --> E. Laparotomy.
◼ Manual de-rotation & check viability.
◼ Viable → Sigmoidopexy.
◼ Gangrenous → Paul-Mickulicz procedure
(or) Hartmann’s operation.
◼ If conditions are good, resection [sigmoid
colectomy] & anastomosis can be done.](https://image.slidesharecdn.com/diverticulosisvolvulusrectalprolapse-250727032604-5de6cd6f/85/Diverticulosis-Volvulus-Rectal-prolapse-pdf-26-320.jpg)



![P R P - TREATMENT
• Digital repositioning – Initially tried.
• Sub-mucosal injections – 10ml of 5%
phenol in almond oil ↓ GA / > 6 weeks.
• Surgery – Thiersch wiring can be tried.
INFANTS / CHILDREN
ADULTS
• Sub-mucosal injections are tried.
• Unilateral - Excision of redundant mucosa
[Goodsall’s Operation]
• Circumf. - Endo-stapling method is used.](https://image.slidesharecdn.com/diverticulosisvolvulusrectalprolapse-250727032604-5de6cd6f/85/Diverticulosis-Volvulus-Rectal-prolapse-pdf-35-320.jpg)

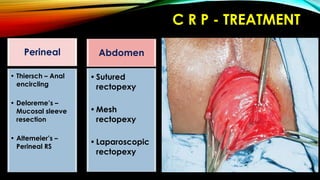
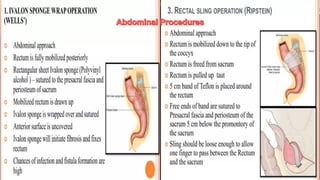
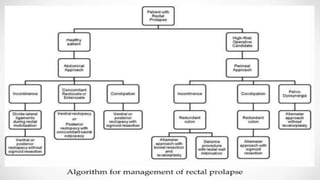
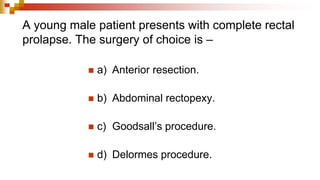
![C R P – AIM - TREATMENT
• To control the prolapse; to restore continence; to
prevent constipation [Perineal / Abdominal].
• Choice of procedure depends on age, sex, operative
risk, pelvic floor defect, degree of incontinence, history
of constipation.
• In young males, abdominal repair should be avoided
as it injures pelvic nerves leading to sexual impotency.
• When the patient is elderly and very frail a perineal
operation is usually safer.](https://image.slidesharecdn.com/diverticulosisvolvulusrectalprolapse-250727032604-5de6cd6f/85/Diverticulosis-Volvulus-Rectal-prolapse-pdf-44-320.jpg)