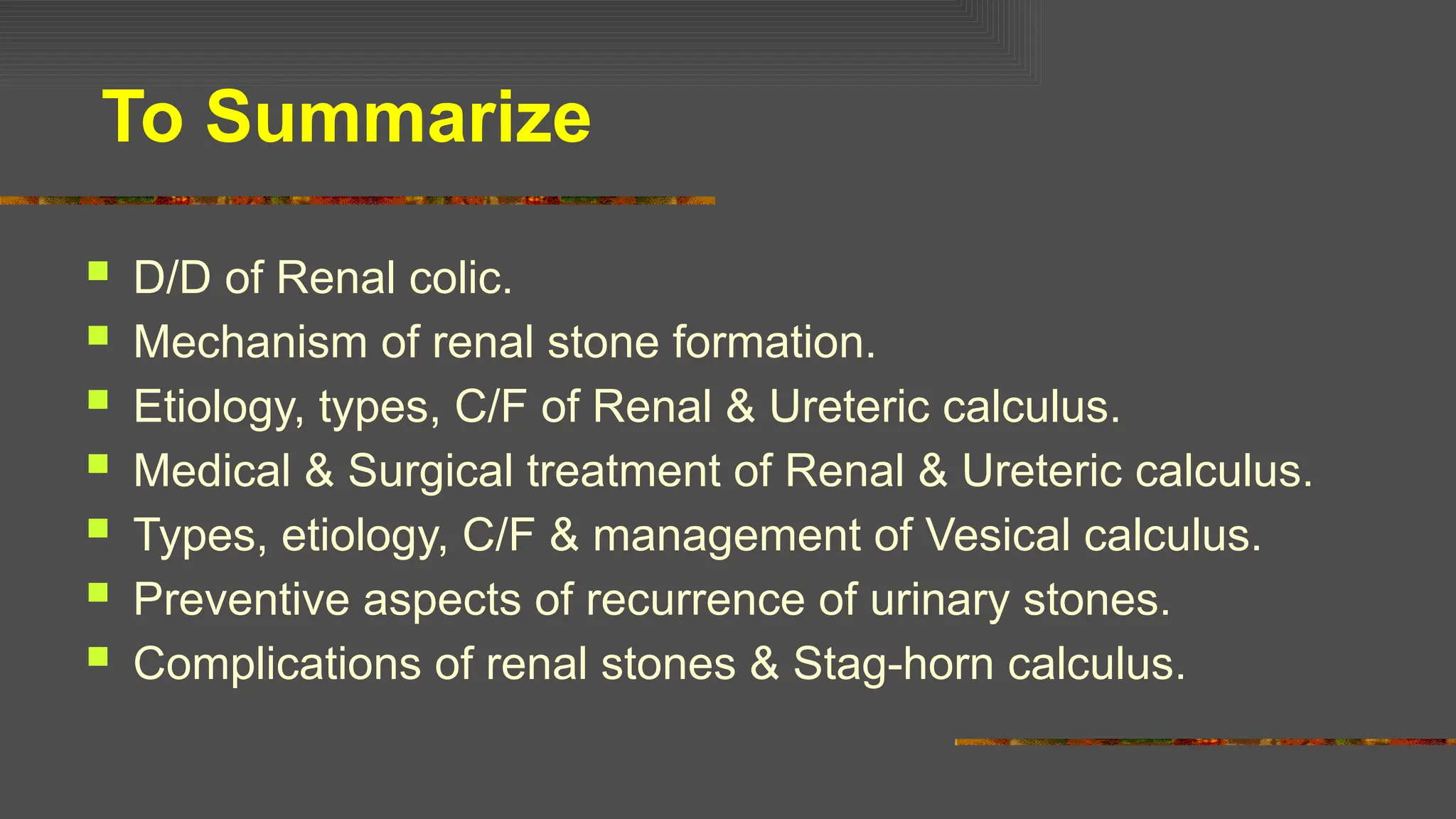
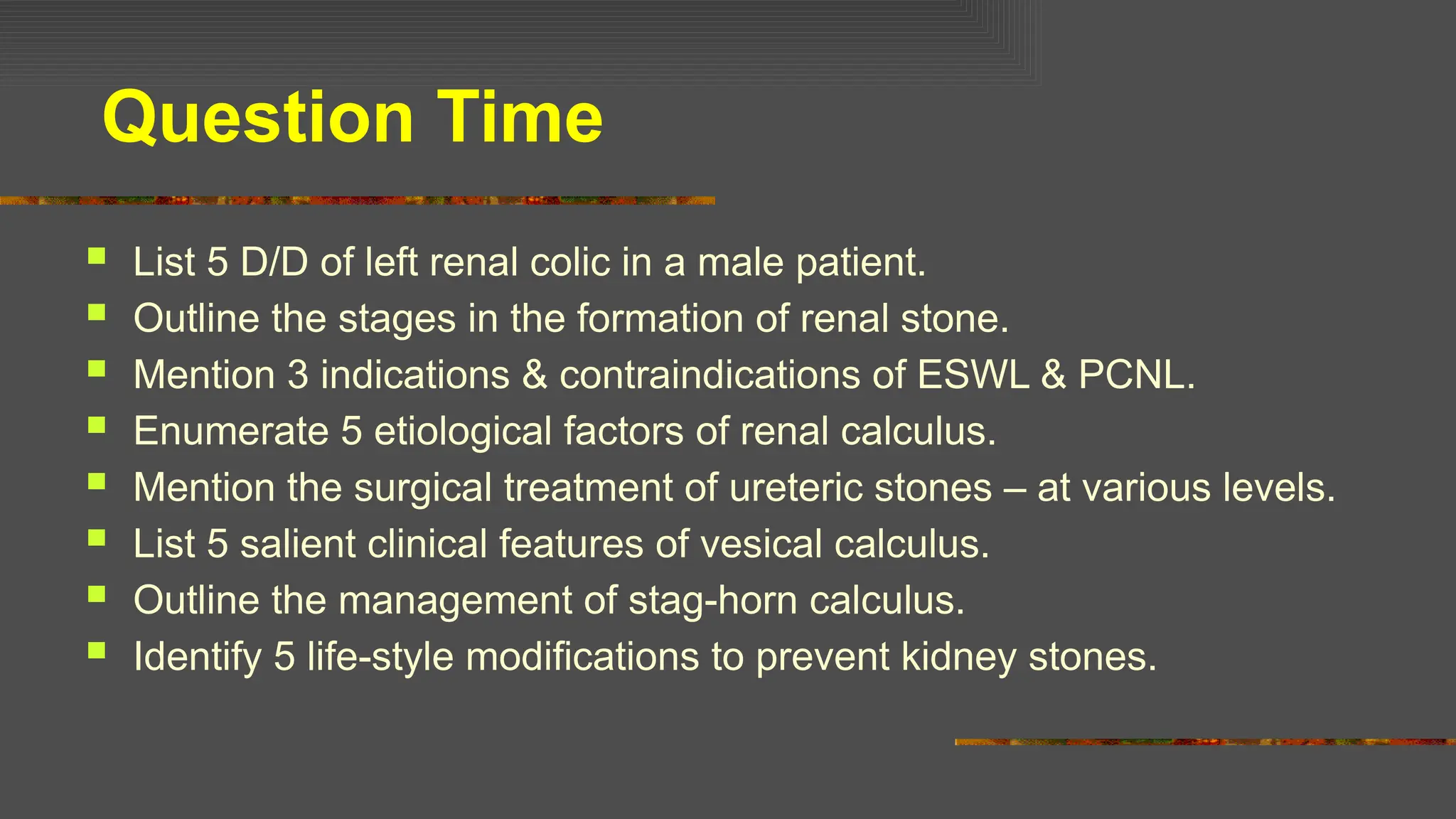
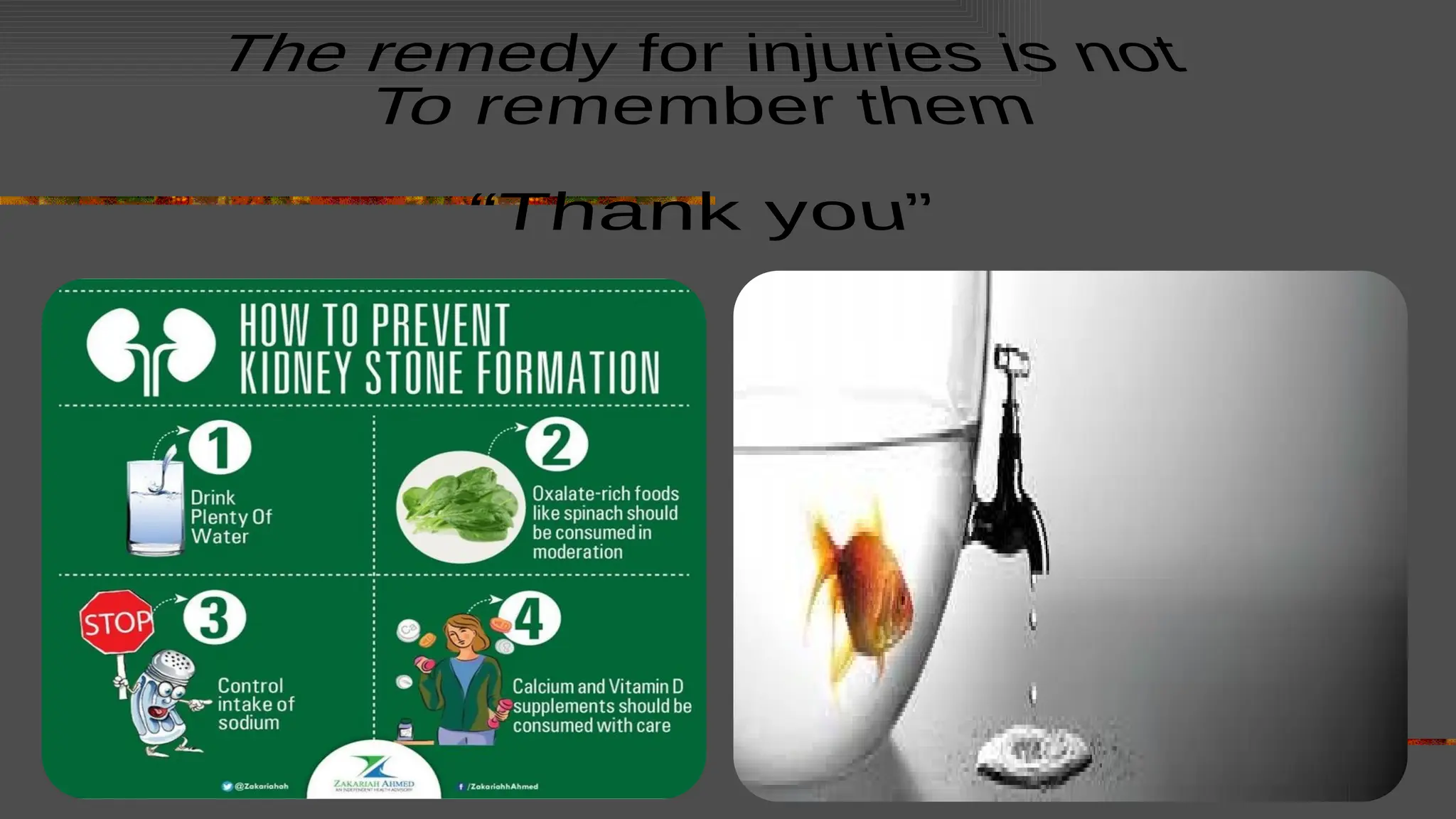
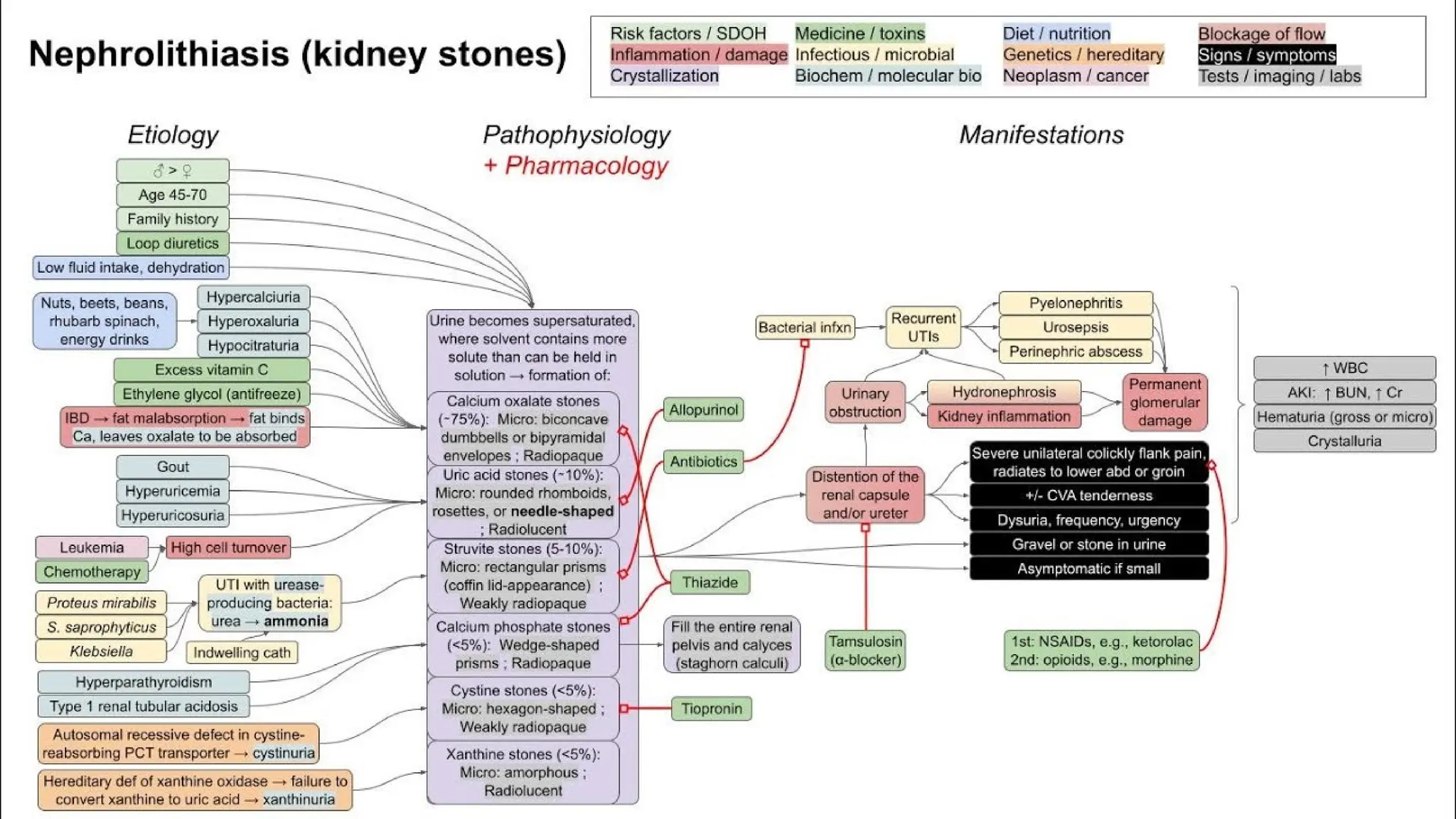
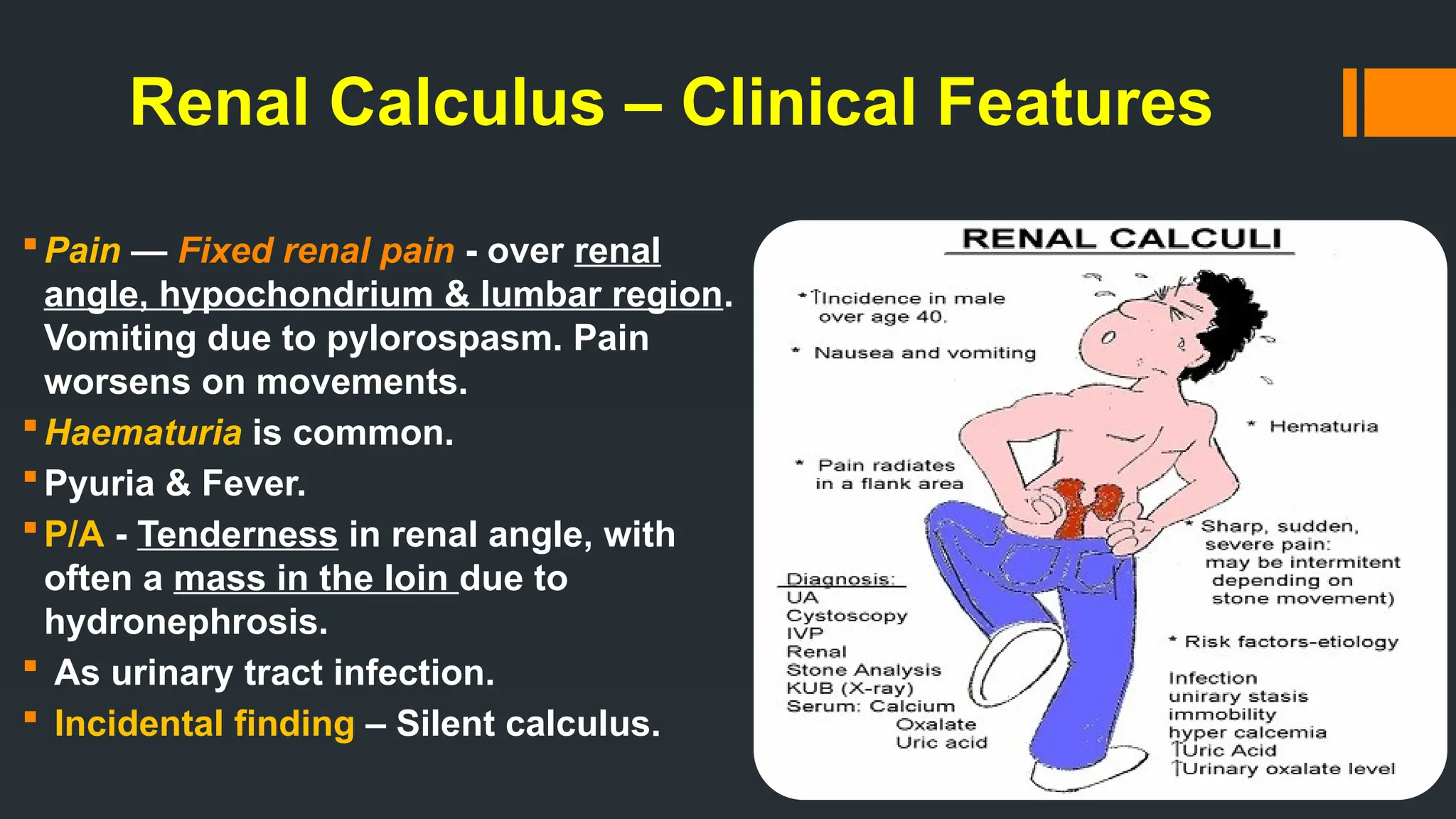
This topic is very important for MBBS - Students....as they are one of the common causes of Acute Abdomen. The students should know the types of renal calculus and their presentation in patients. Also, when to go for conservative treatment and when to surgically intervene....They should also know the preventive measures against stone formation....
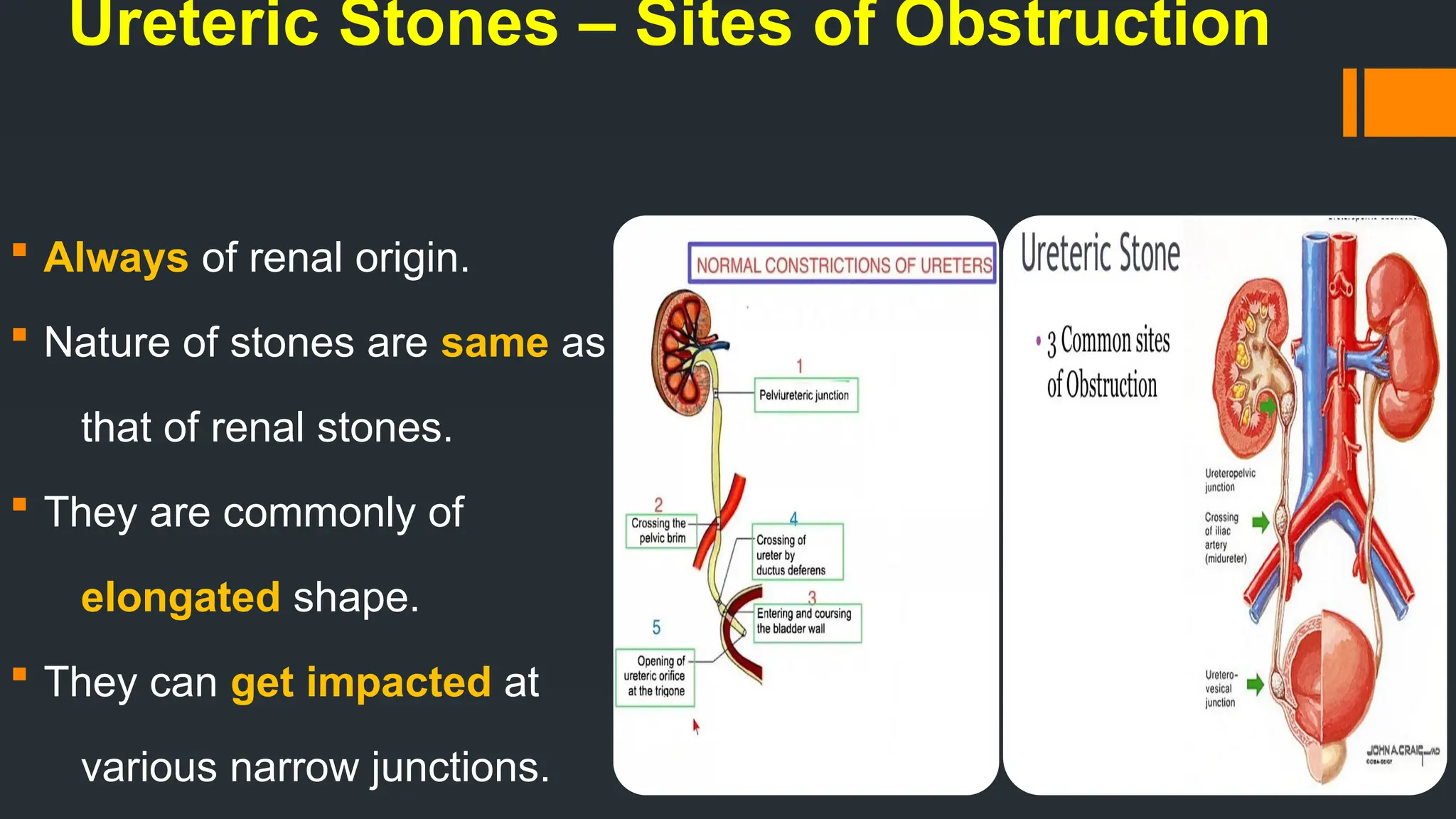
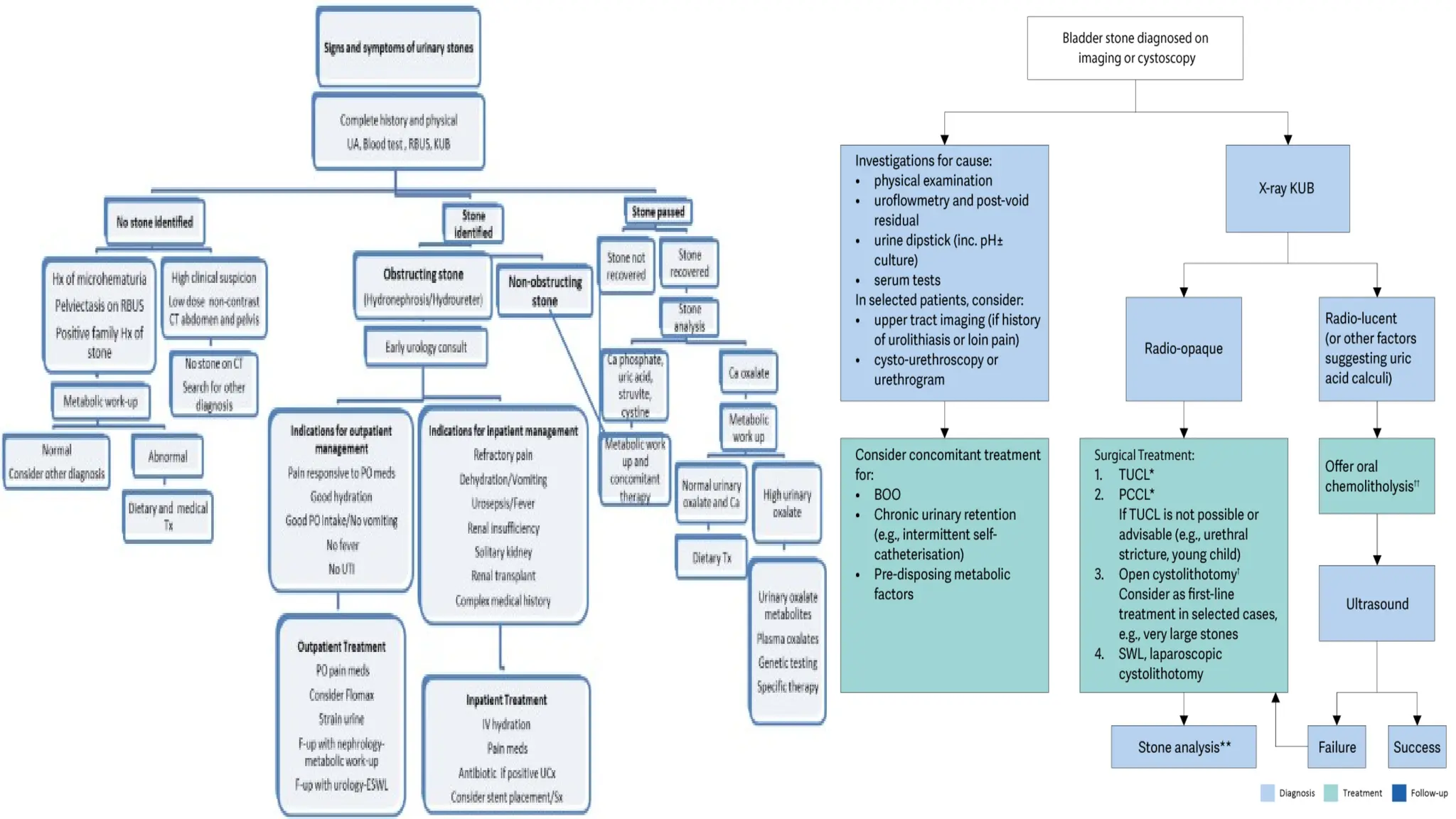
![Ureteric Calculus – C/F
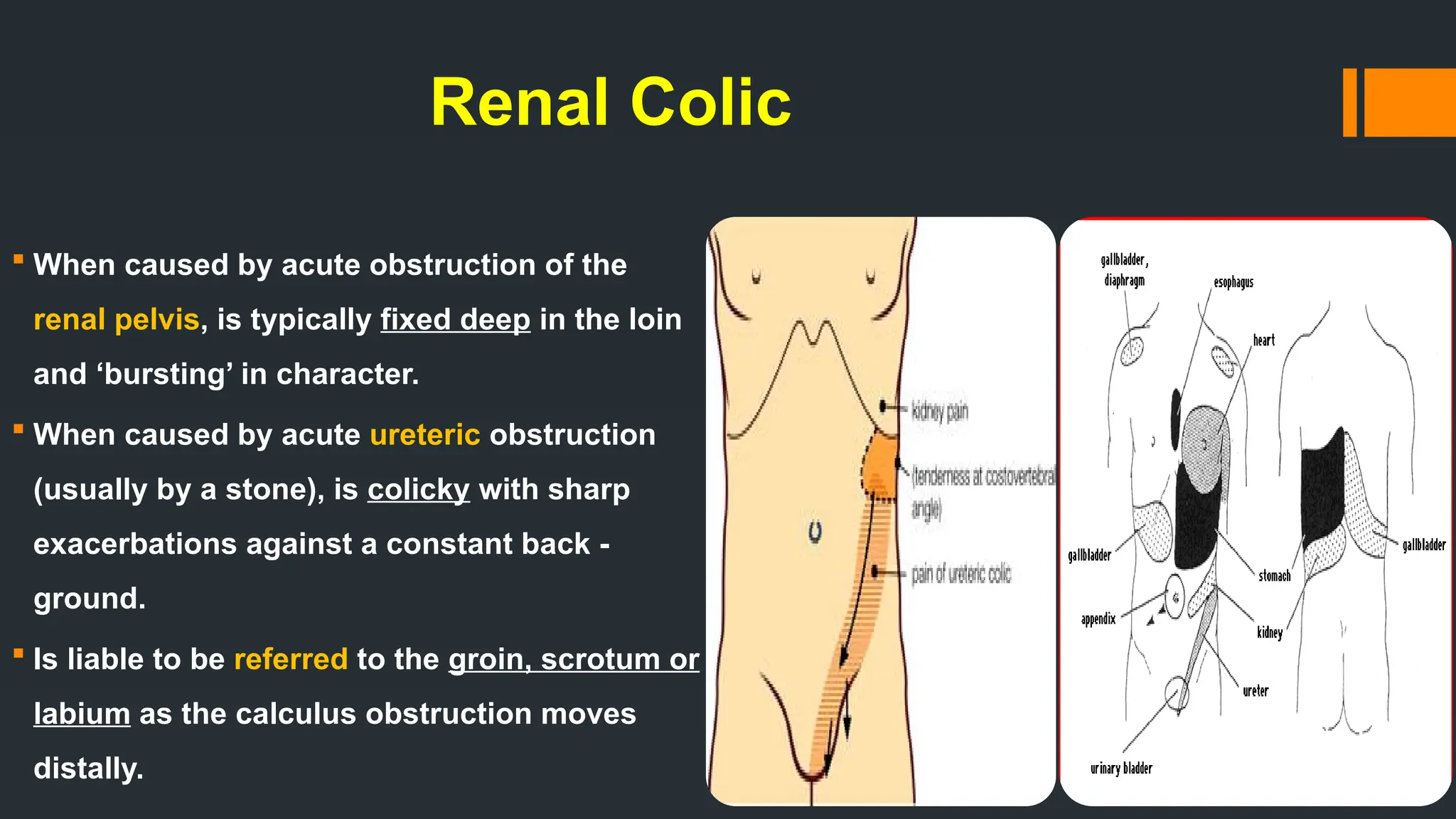
Pain — It is of colicky type and
radiates from loin to groin often to the
tip of the genitalia - testis in males,
labia majora in females [G F N].
It is severe in intensity, increases with
exercise.
Nausea, vomiting, sweating due to
pain and reflex pylorospasm.
Haematuria, dysuria, frequency,
strangury.
Tenderness in over some part of the
course of the ureter - (iliac fossa /
renal angle).](https://image.slidesharecdn.com/urolithiasis-251107120904-cb860b46/75/Urolithiasis-Stones-of-the-Urinary-System-25-2048.jpg)