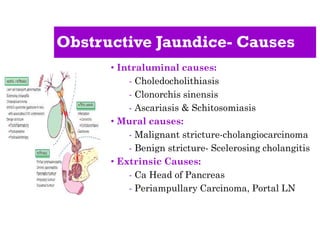
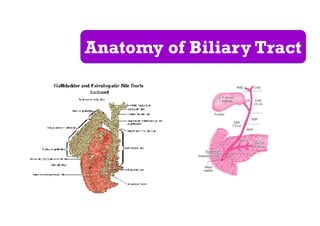
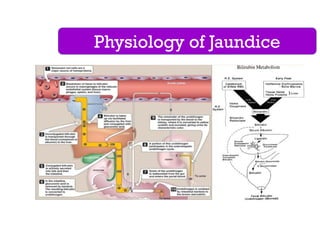
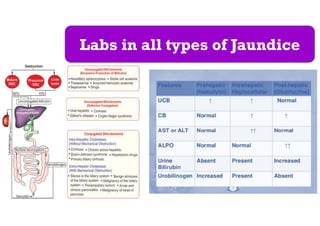
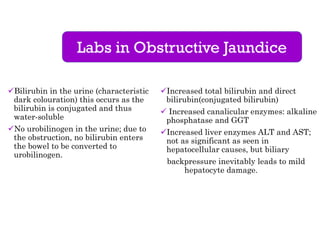
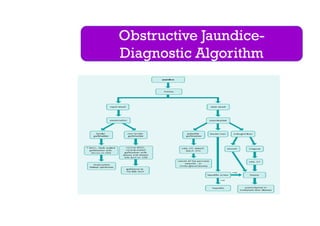
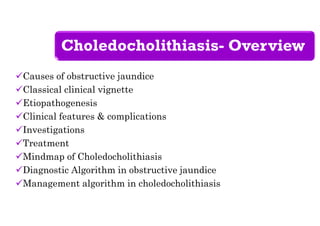
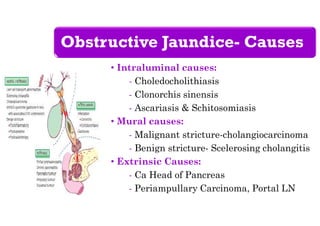
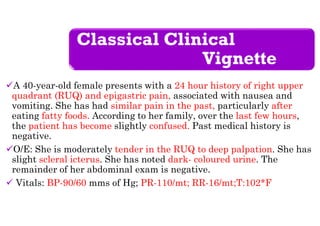
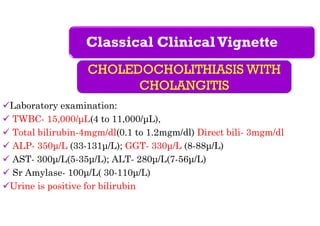
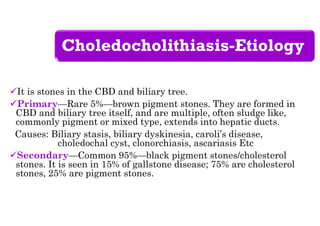
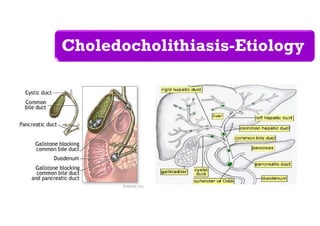
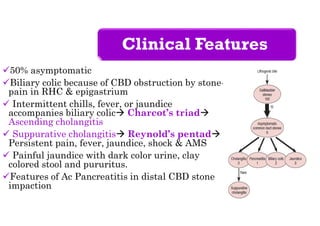
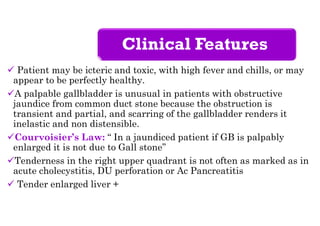
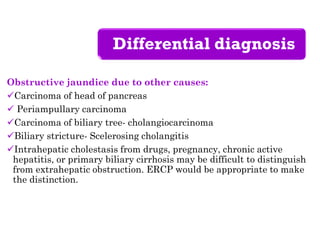
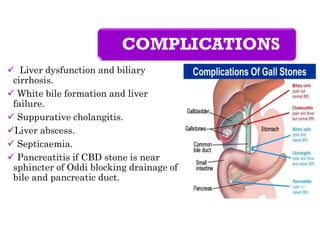
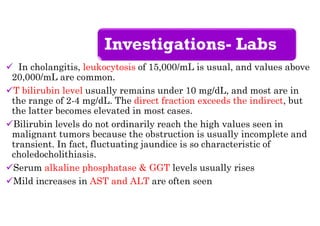
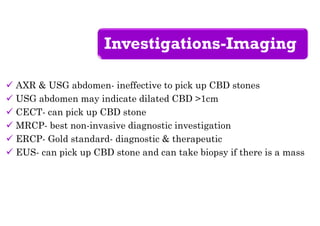
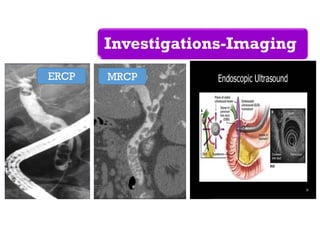
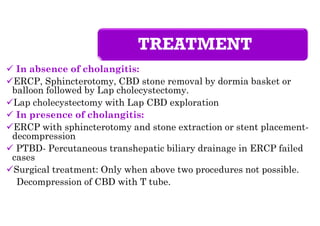
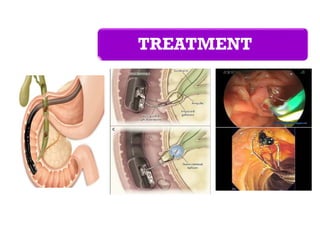
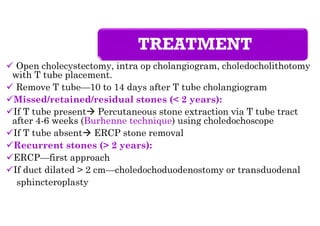
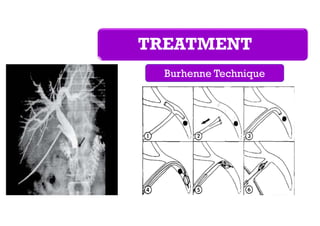
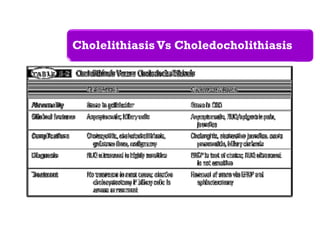
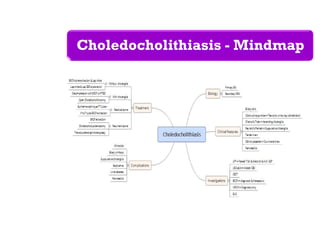
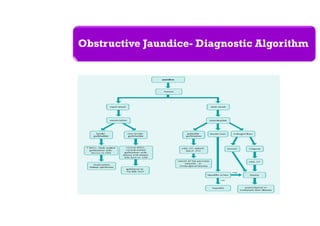
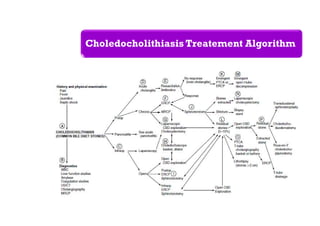
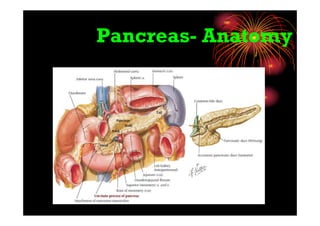
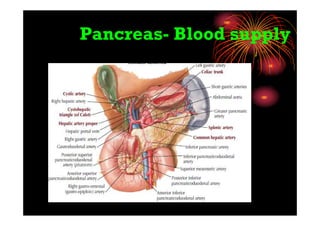
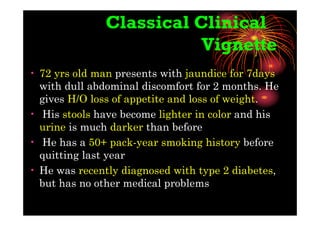
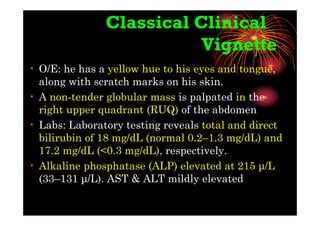
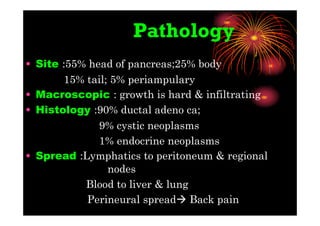
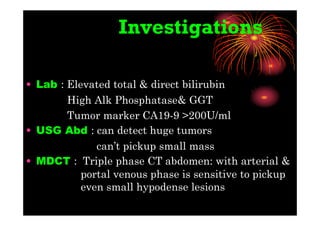
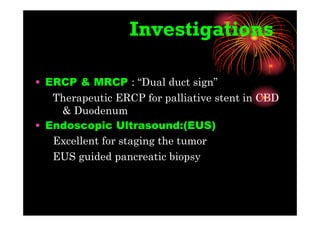
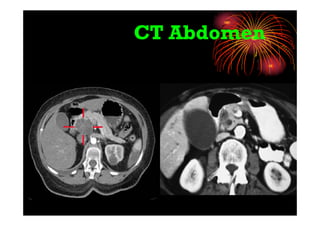
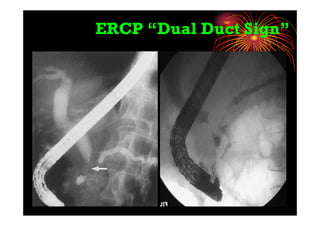
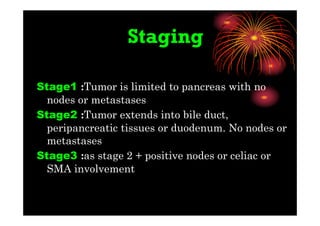
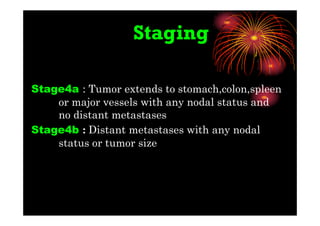
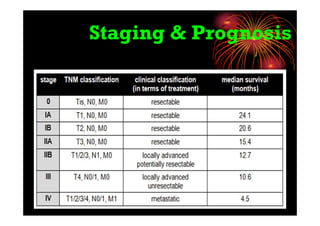
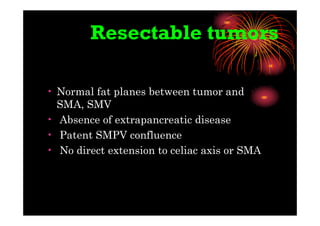
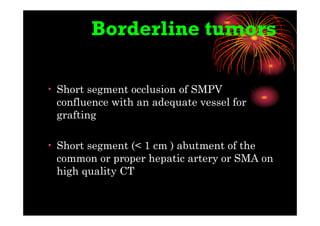
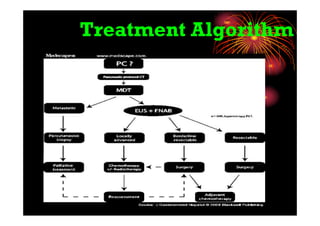
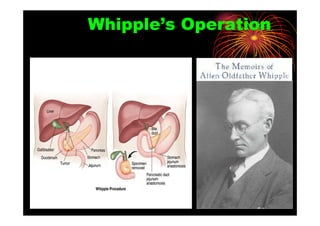
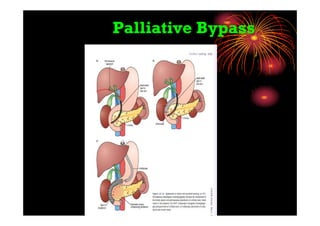
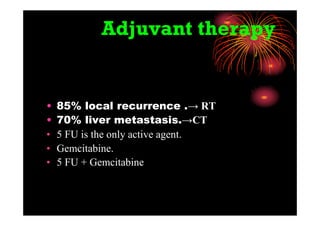
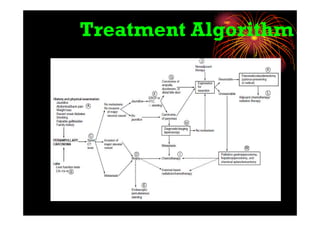
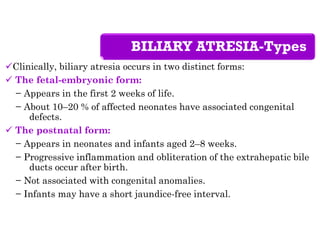
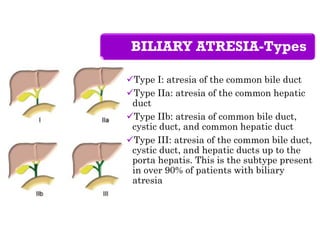
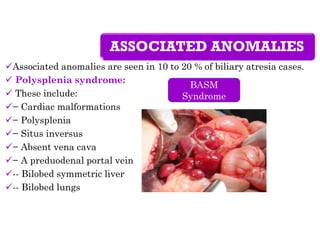
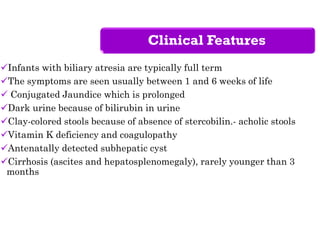
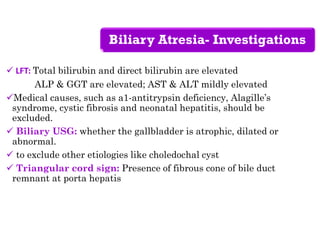
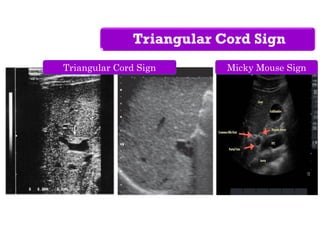
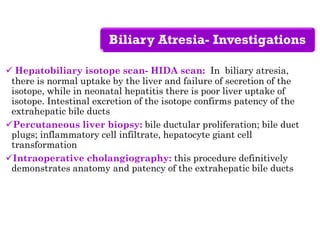
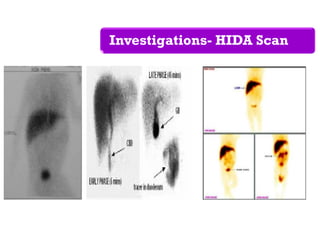
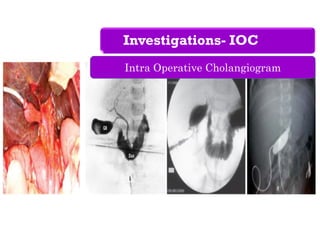
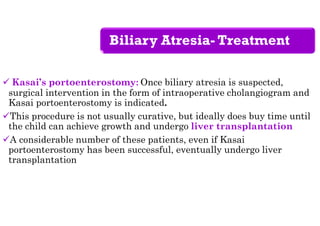
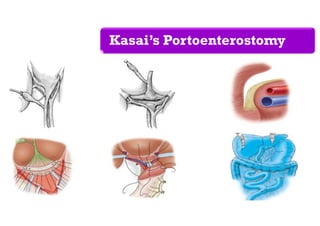
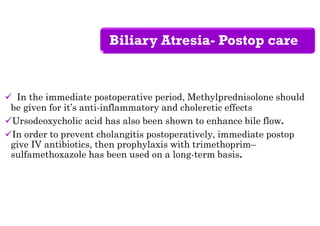
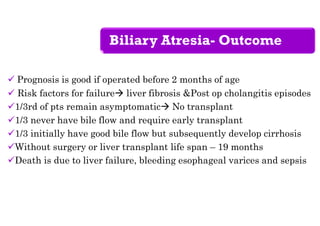
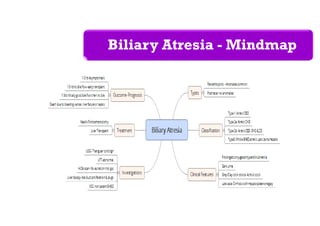
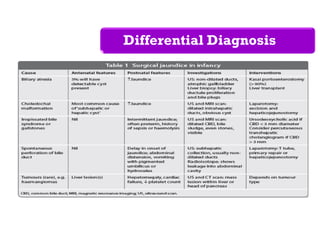
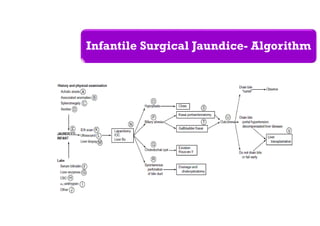
The document provides an extensive overview of obstructive jaundice, including its causes, clinical features, and management options. Key points include intraluminal, mural, and extrinsic causes of obstructive jaundice, with diagnostic approaches such as ERCP and imaging studies emphasized for effective treatment. It details the clinical presentations, investigations, and algorithms for managing conditions like choledocholithiasis and pancreatic carcinoma, as well as understanding biliary atresia in infants.