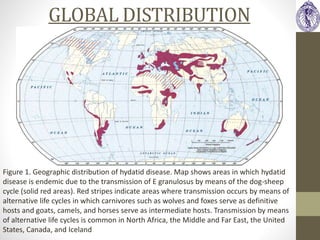
An 26-year-old female presented with abdominal pain, hepatomegaly, and fever. Imaging revealed hepatic cysts, with differential diagnoses including cystic echinococcosis. Cystic echinococcosis is caused by the tapeworm Echinococcus granulosus and is endemic in pastoral communities. It involves the growth of cysts, most commonly in the liver and lungs, which can cause complications as they increase in size. Diagnosis involves serology, imaging, and cyst puncture. Treatment options include benzimidazole medication, percutaneous cyst sterilization, surgery, or observation of asymptomatic cysts. Prevention requires reducing transmission between definitive canine hosts and intermediate livestock hosts.



![DIFFERENTIAL DIAGNOSIS
HEPATIC SAPCE
OCCUPYING LESIONS
Cystic/Pseudocystic
Space-Occupying Lesions
with Liquid Content
Solid Space-Occupying
Lesions
CONGENITAL SPACE-
OCCUPYING LESIONS
Simple cyst Haemorrhagic simple
cyst
VASCULAR SPACE-
OCCUPYING LESIONS
Haematoma Haematoma
Haemangioma
INFECTIOUS SPACE-
OCCUPYING LESIONS
CE [CE1, CE2, CE3a,
CE3b (mixed cystic-
solid)]
AE with pseudocyst
Abscess
CE [CE3b (mixed cystic-
solid),
CE4 and CE5]
AE
Tuberculoma
BENIGN SPACE-
OCCUPYING LESIONS
Cystadenoma Hepatic adenoma
Focal nodular
hyperplasia
MALIGNANT SPACE-
OCCUPYING LESIONS
Cystadenocarcinoma
Liver metastases with
central necrosis
Metastatic liver tumours
Hepatocellular
carcinoma
Cholangiocarcinoma](https://image.slidesharecdn.com/hydatiddisease-160512160555/85/Hydatid-diseases-6-320.jpg)










![INVESTIGATIONS
LABORATORY WORK UP:
• Routine lab tests: No specific findings
• Cyst rupture in biliary tree: marked & transient elevation of
cholestatic enzyme levels , often with hyperamylasemia and
eosinophilia <15% (in 60% cases)
• SEROLOGY: Confirmatory role; Indirect hemagglutination test
& ELISA for detection of anti-Echinococcus Antibodies [IgG]
• 10% hepatic cysts & 40% pulmonary cysts exhibit false
negative results
-ve in CE1/CE2/CE4/CE5; +ve only when endocyst ruptures
• Diagnostic puncture & aspiration can be performed for
histological diagnosis
• PCR contribute to the differential diagnosis between CE and
AE in doubt.](https://image.slidesharecdn.com/hydatiddisease-160512160555/85/Hydatid-diseases-18-320.jpg)