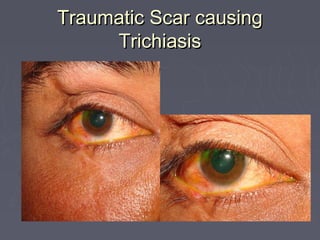
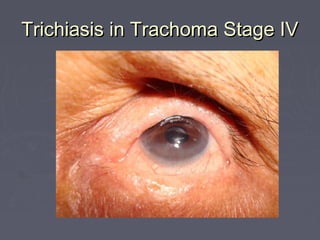
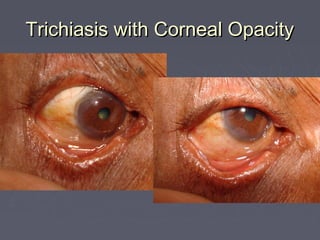
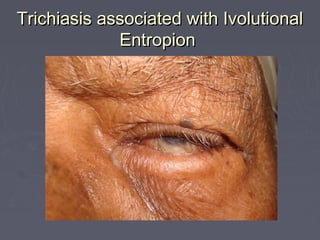
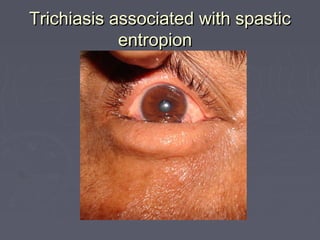
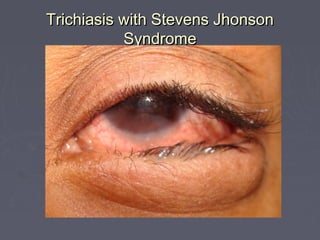
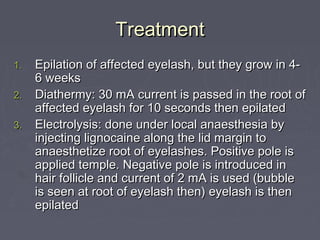
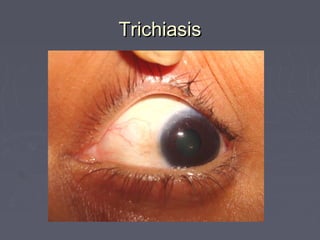
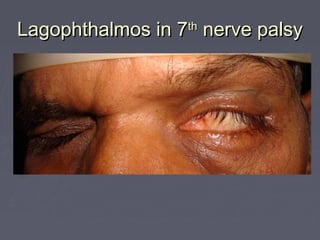
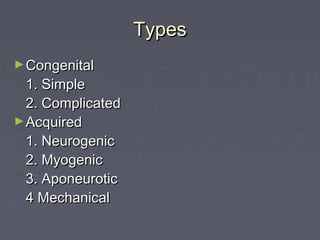
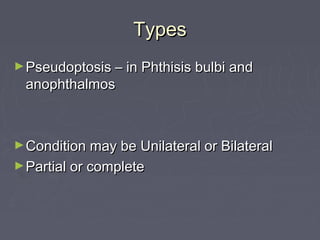
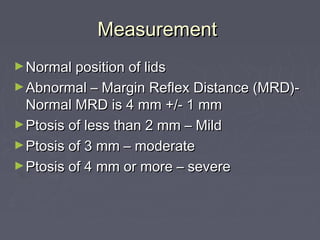
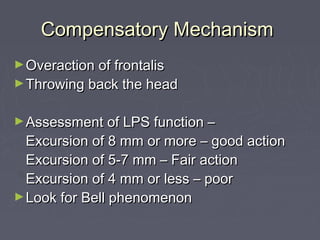
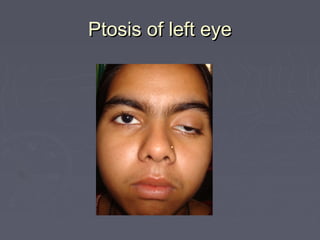
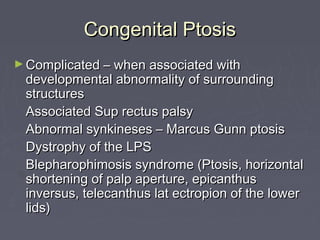
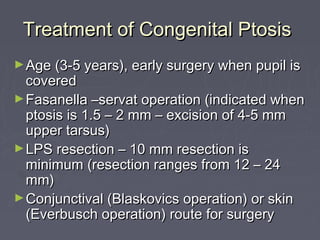
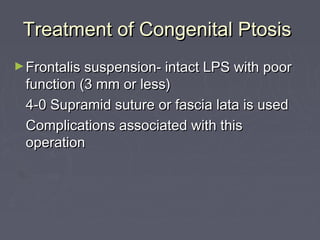
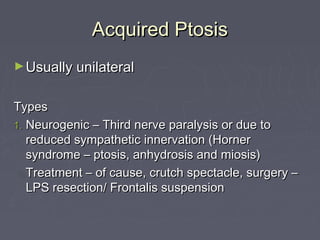
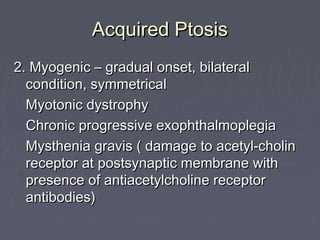
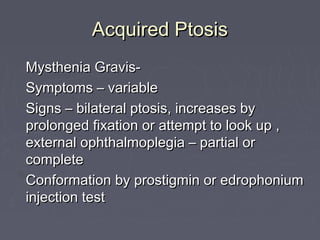
Trichiasis is a condition characterized by misdirected eyelashes that rub against the cornea. It can be caused by entropion due to conditions like trachoma or scarring. Symptoms include irritation, pain, and blurred vision. Treatment options include epilation, cryotherapy, or electrolysis to remove misdirected eyelashes. Lagophthalmos is incomplete eye closure that can result from lid paralysis or contraction. It puts the cornea at risk for drying and infection if not treated with lubricants, taping, or tarsorrhaphy surgery. Ptosis refers to drooping of the upper eyelid and can be congenital, neurogenic, myogenic, or involutional in nature. The