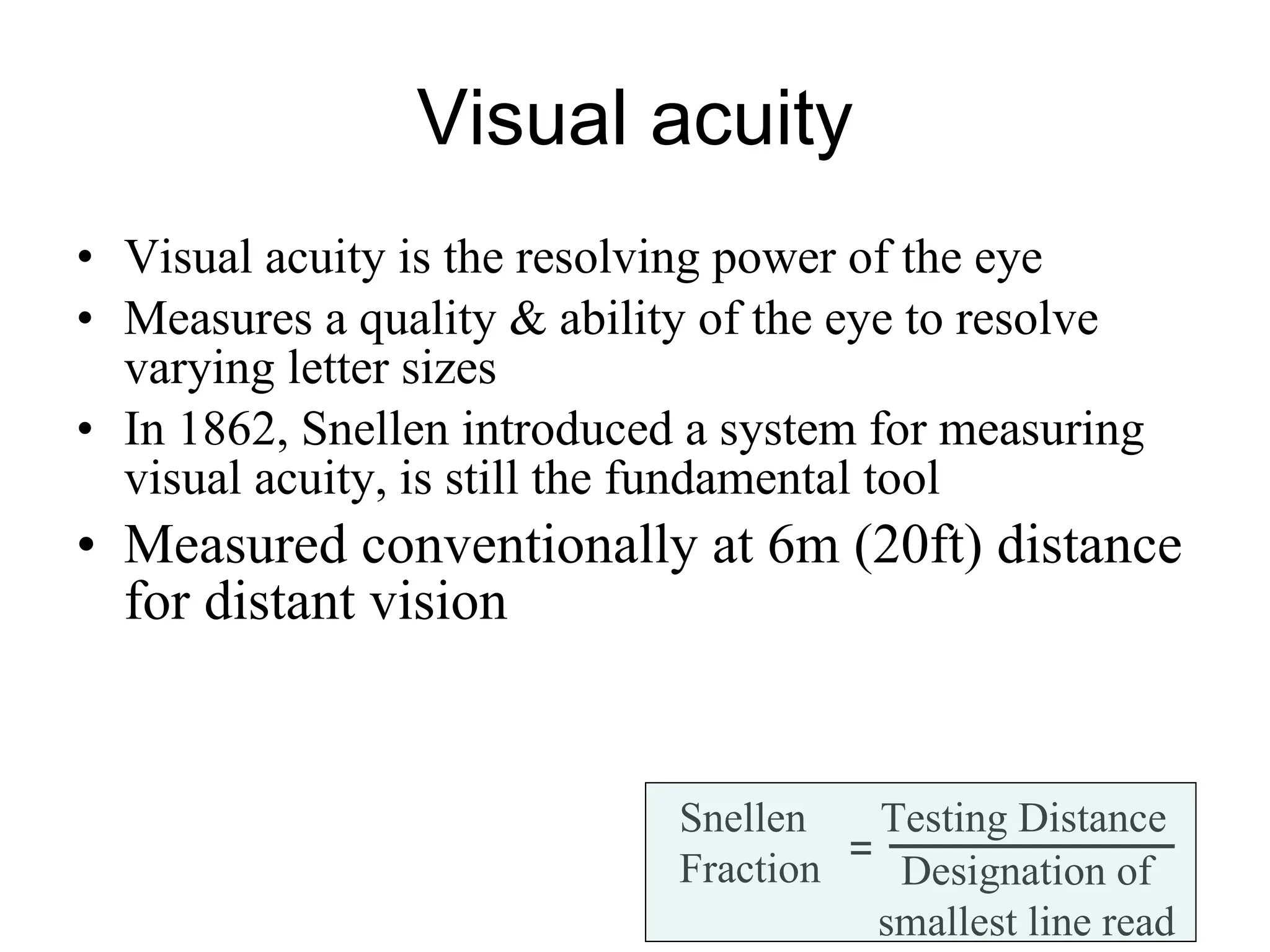
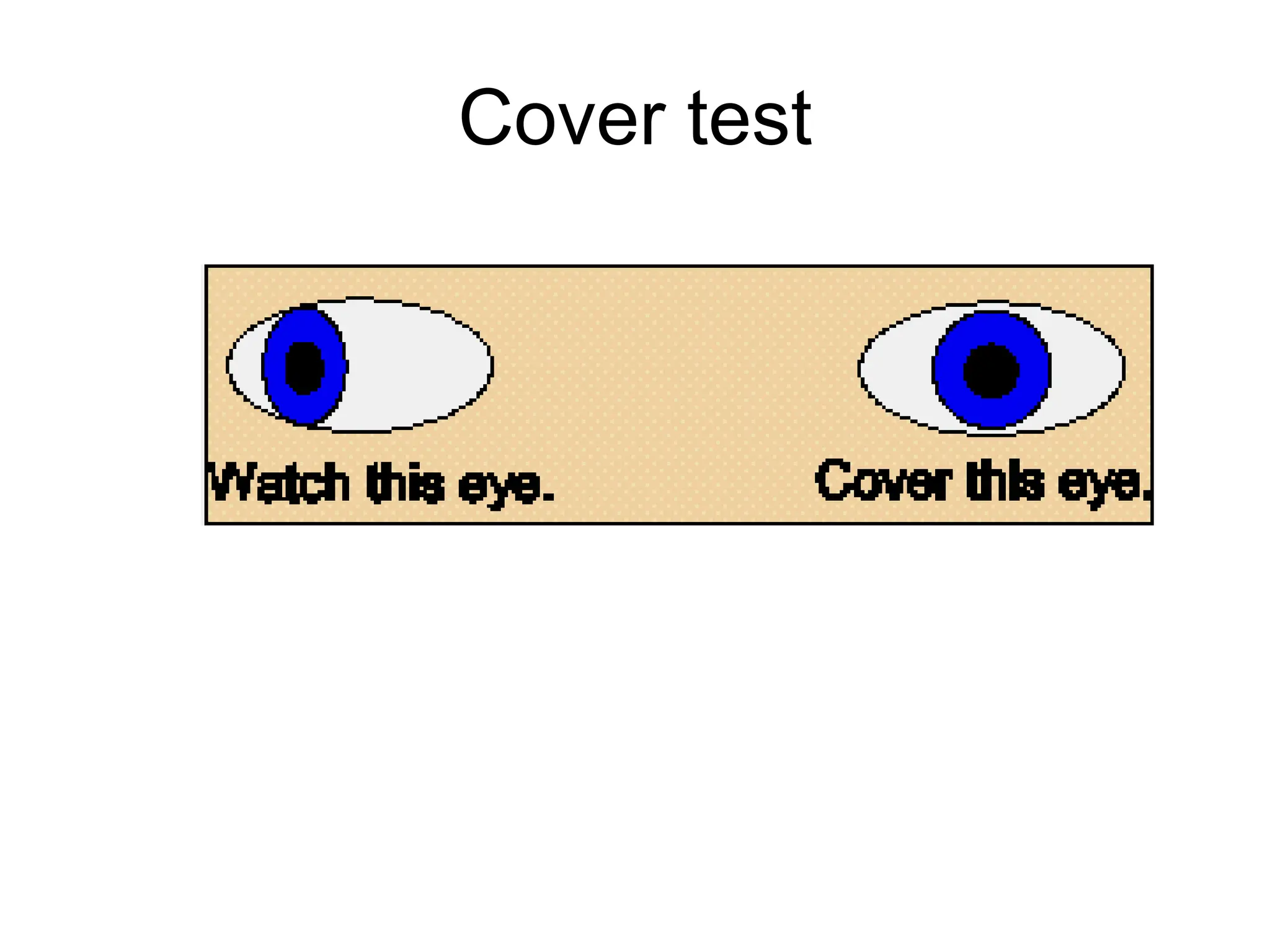
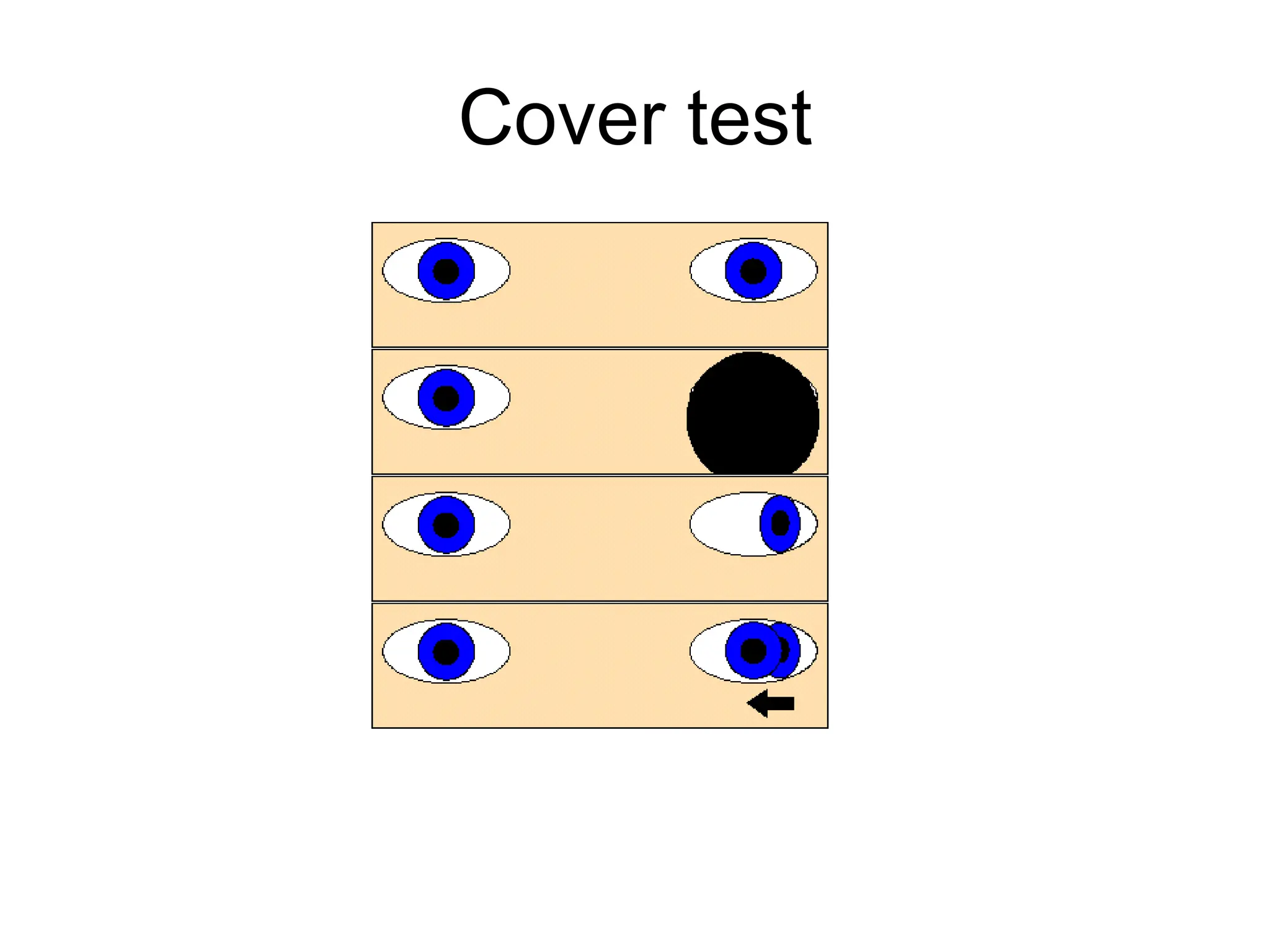
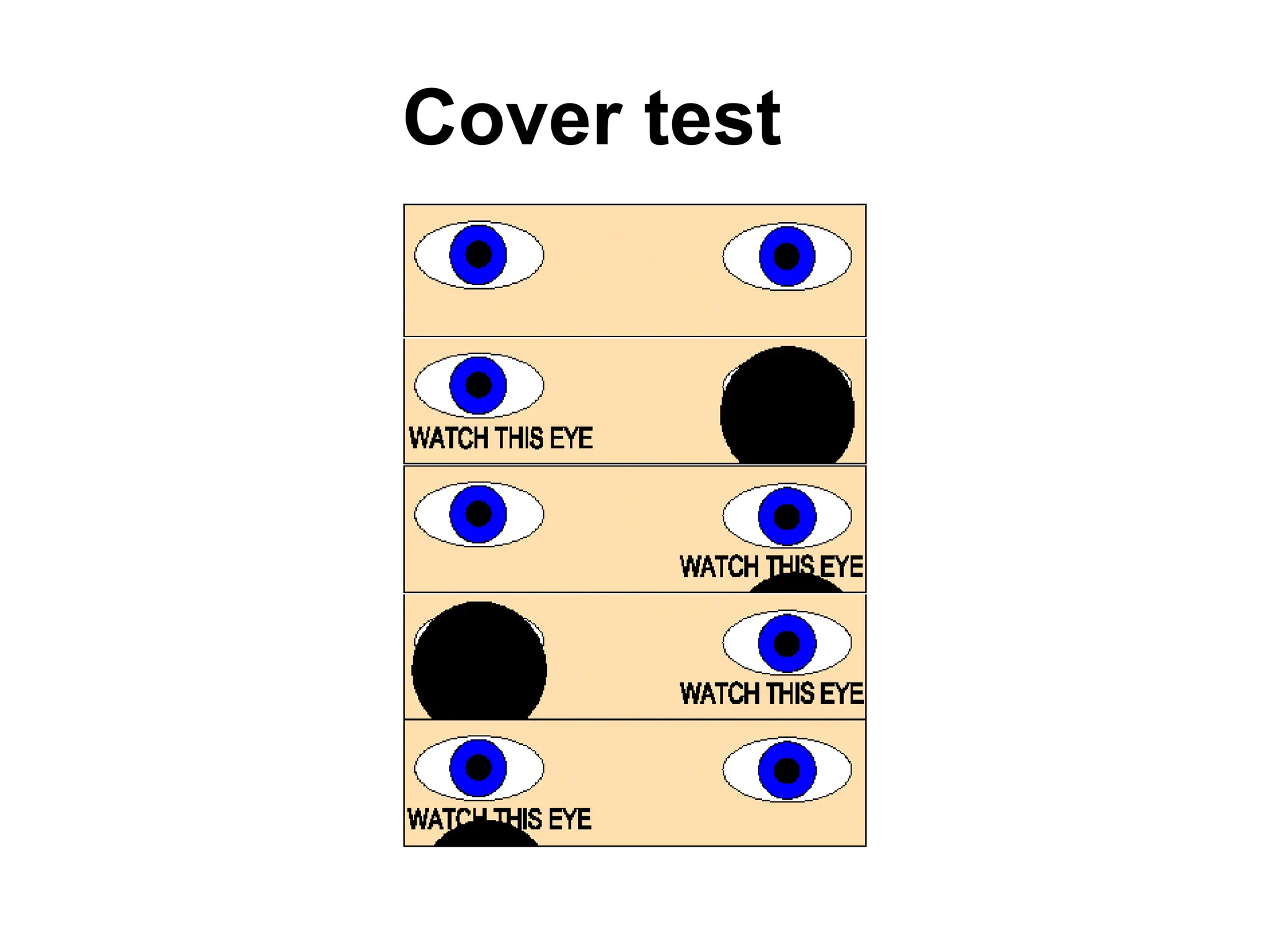
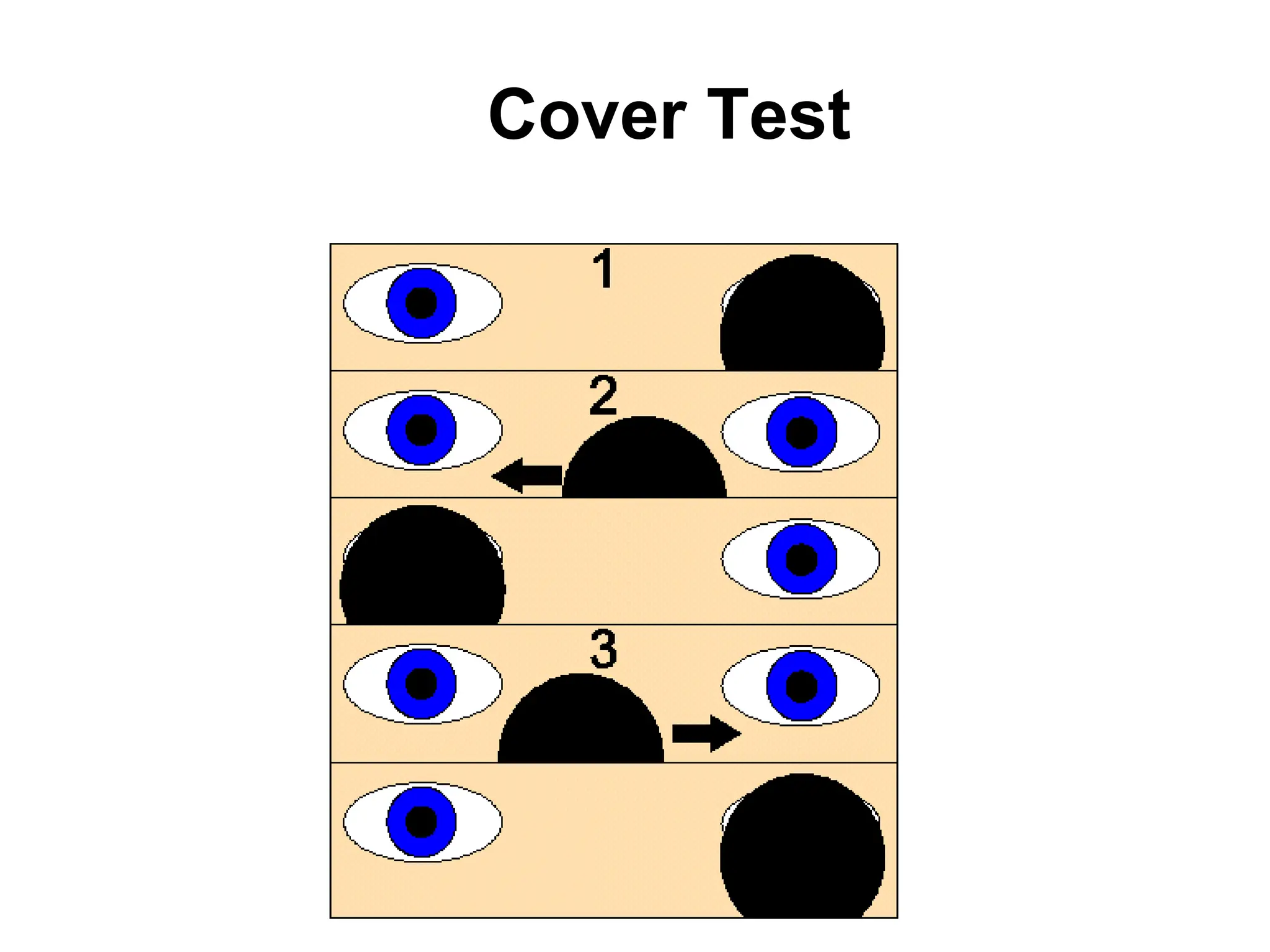
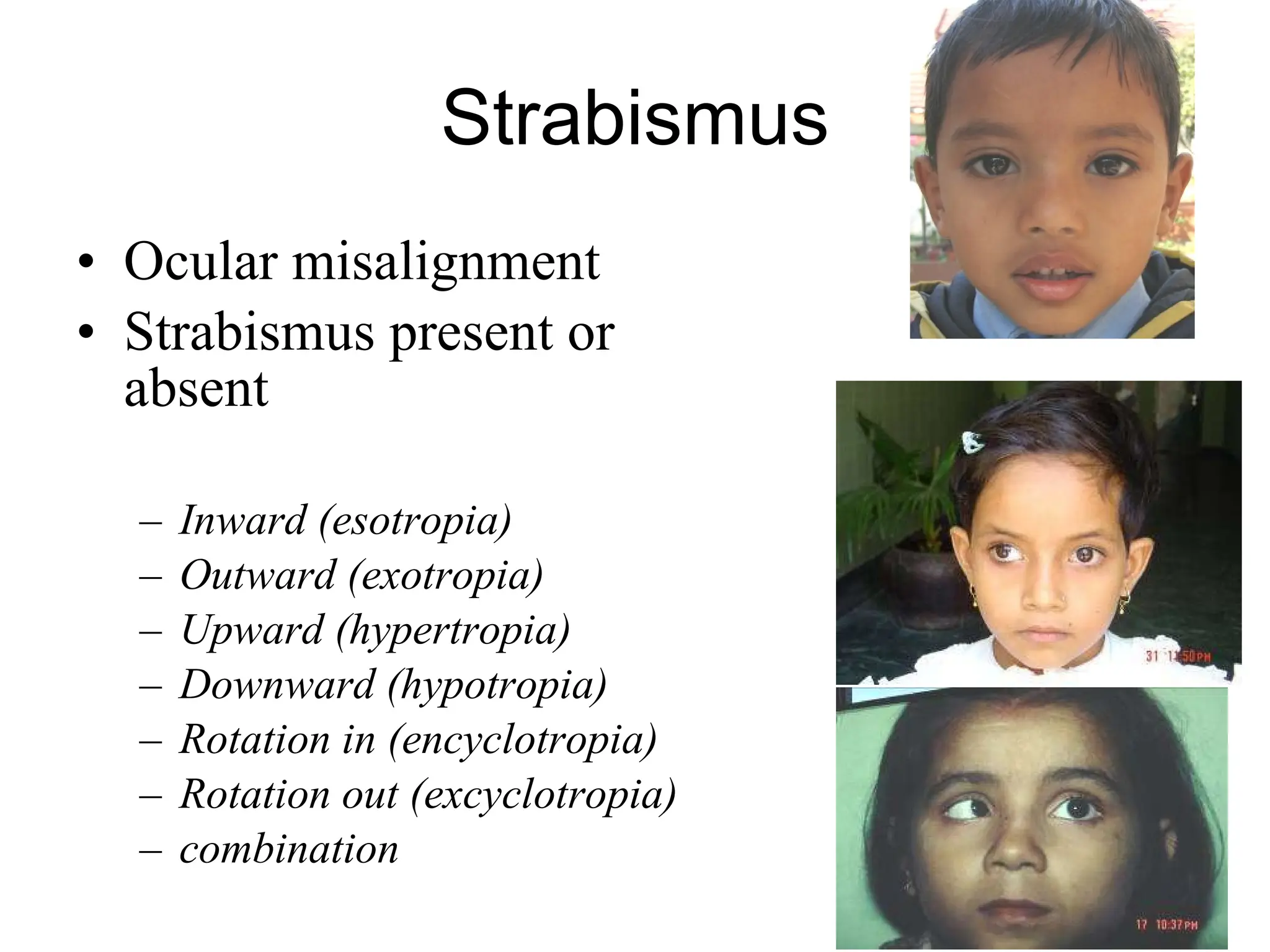
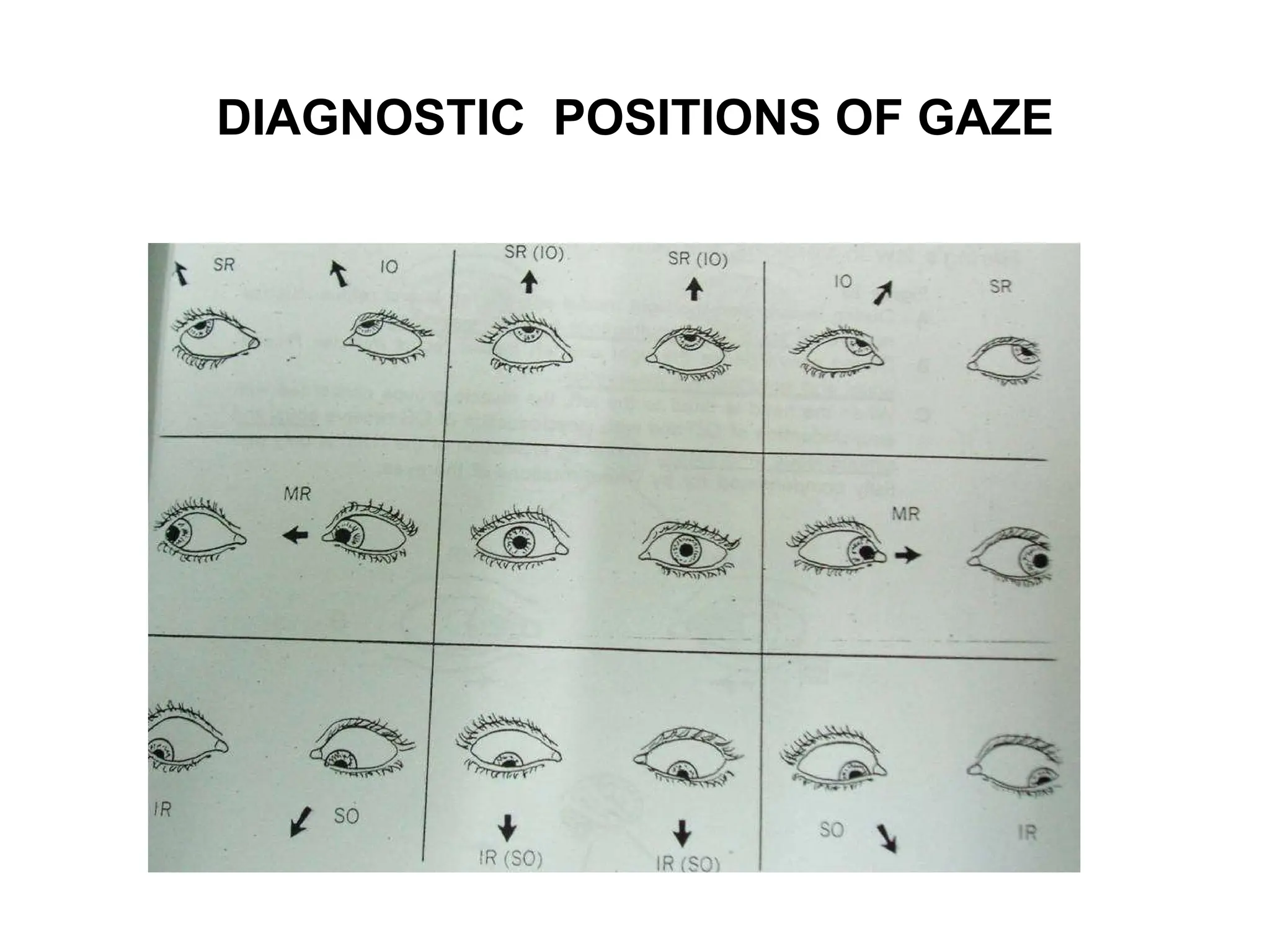
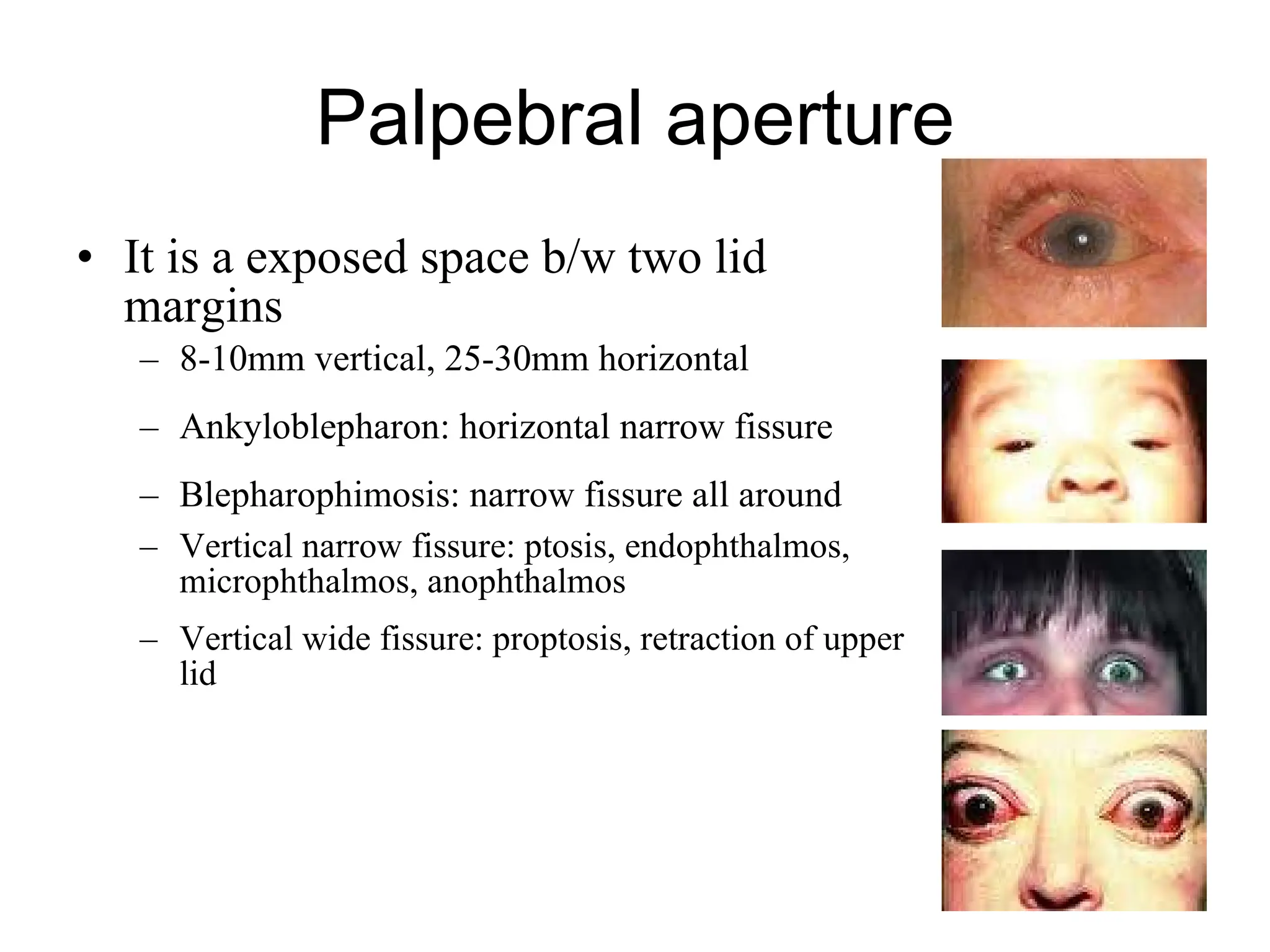
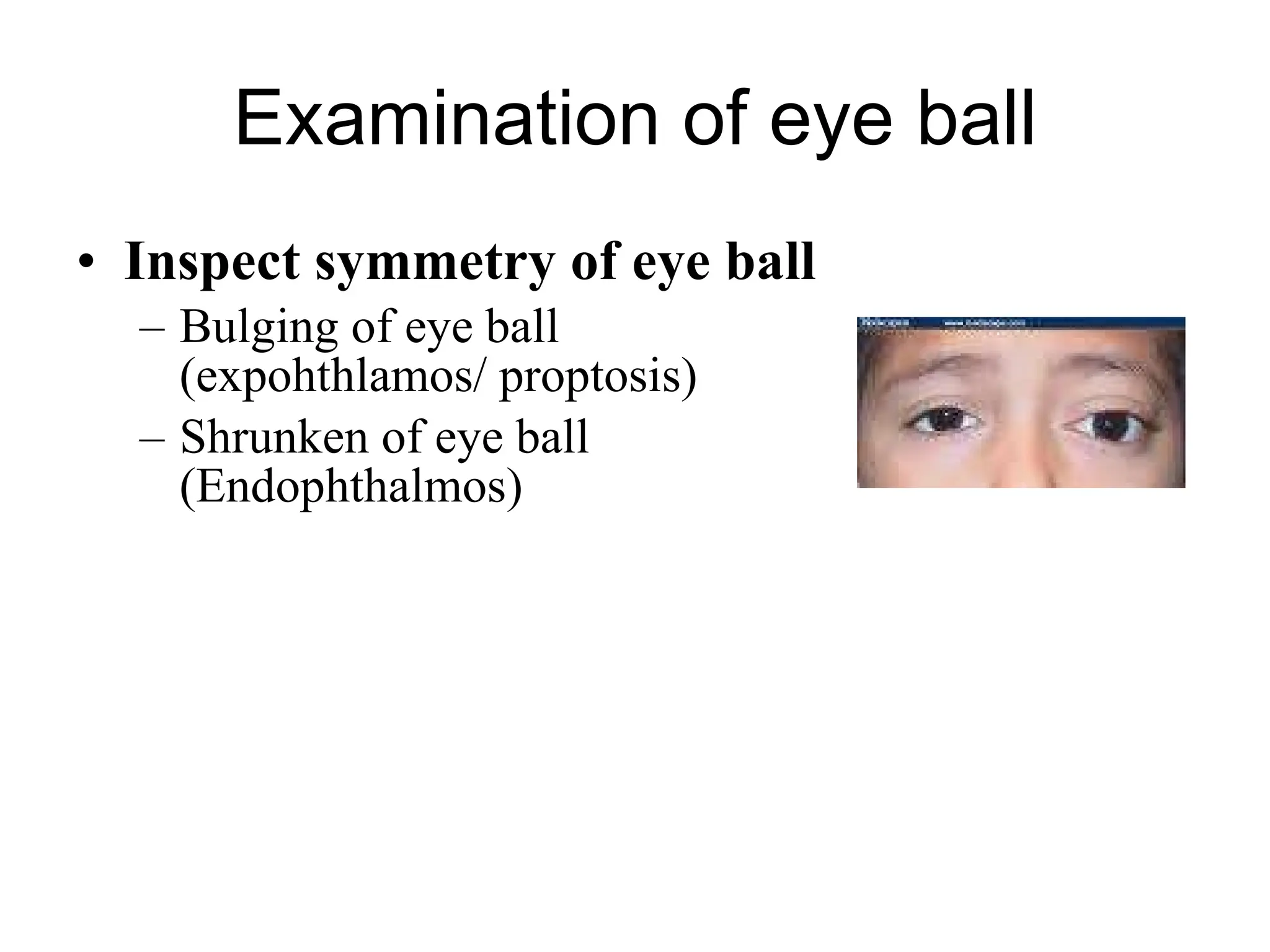
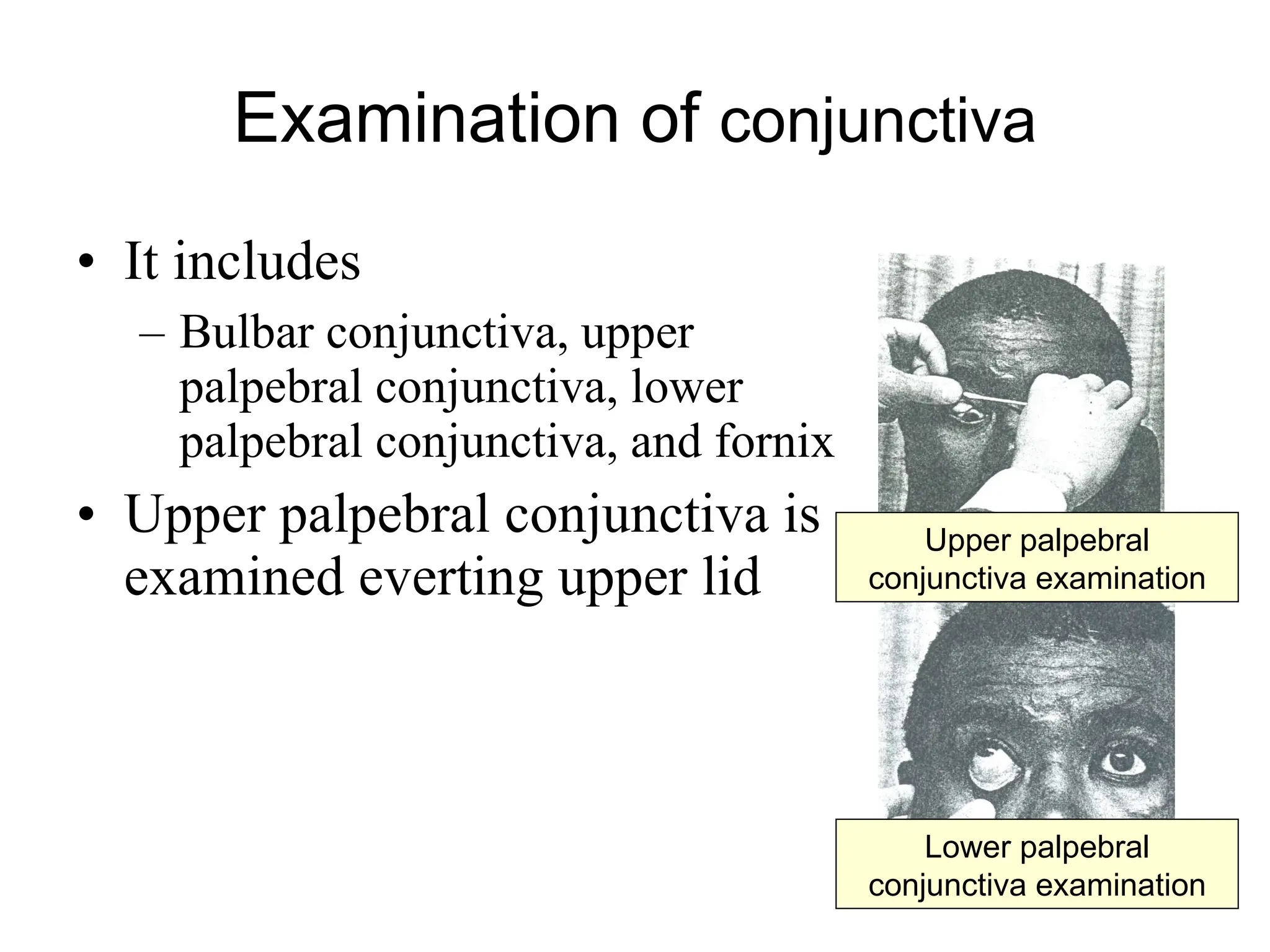
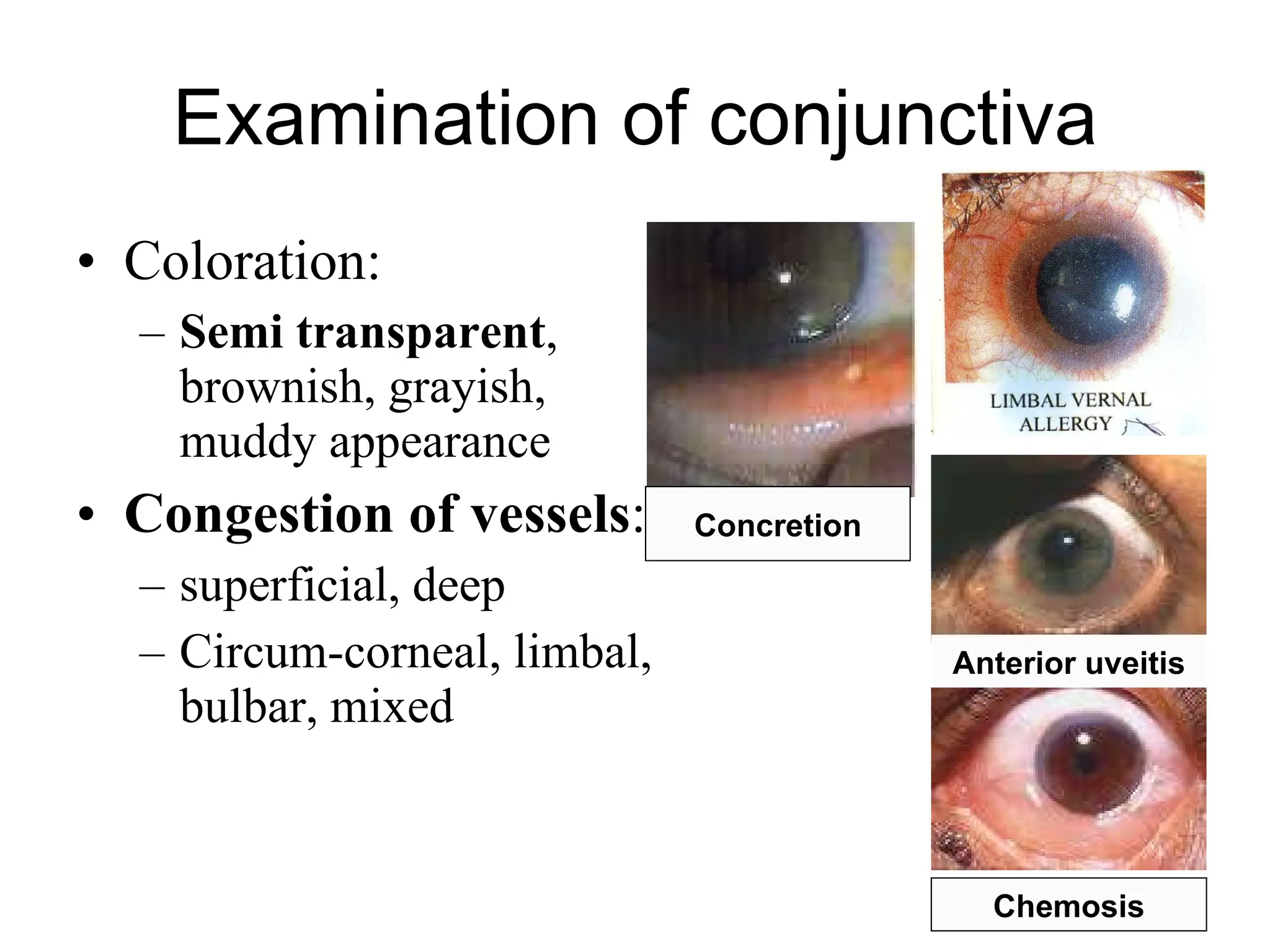
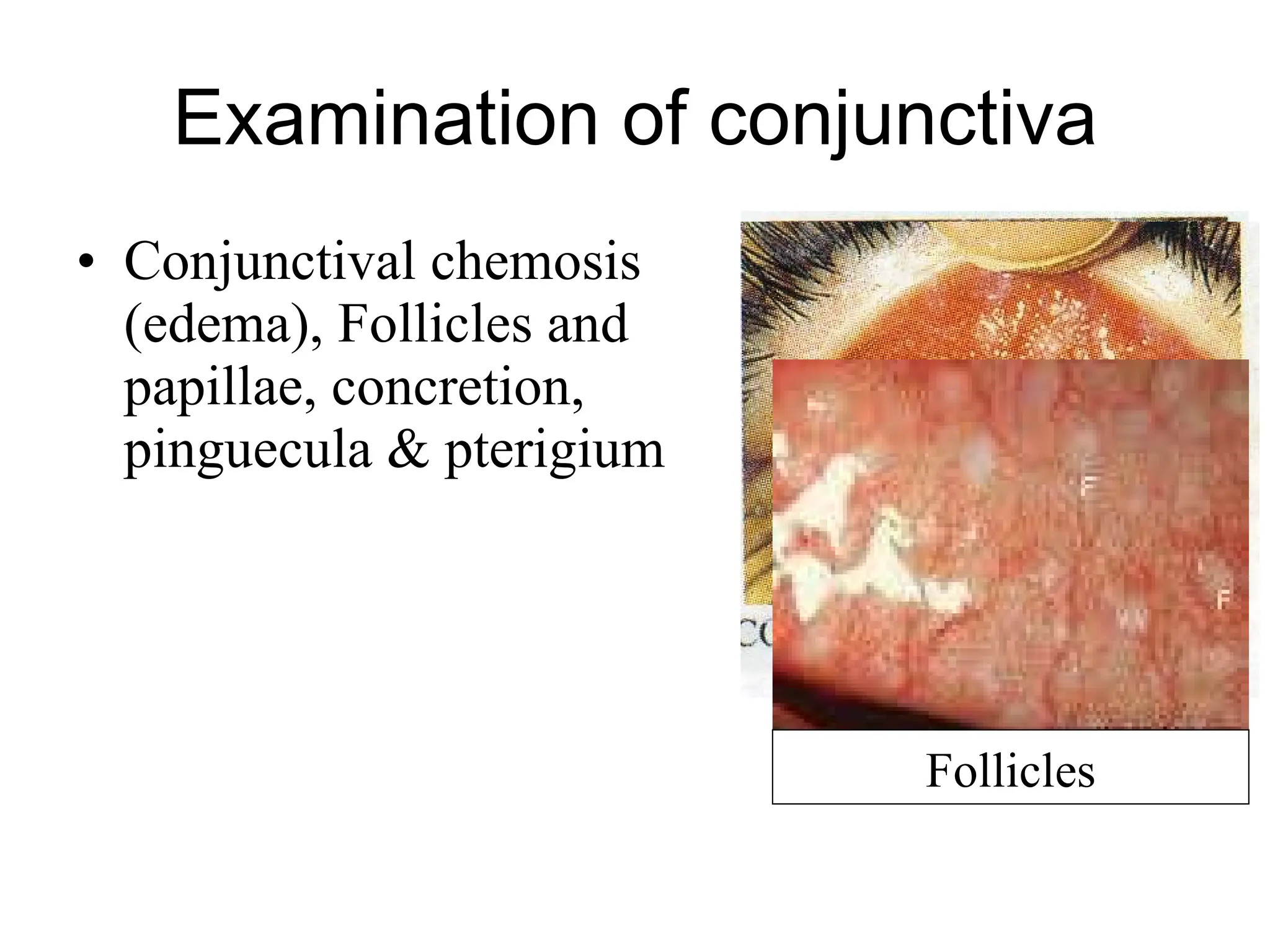
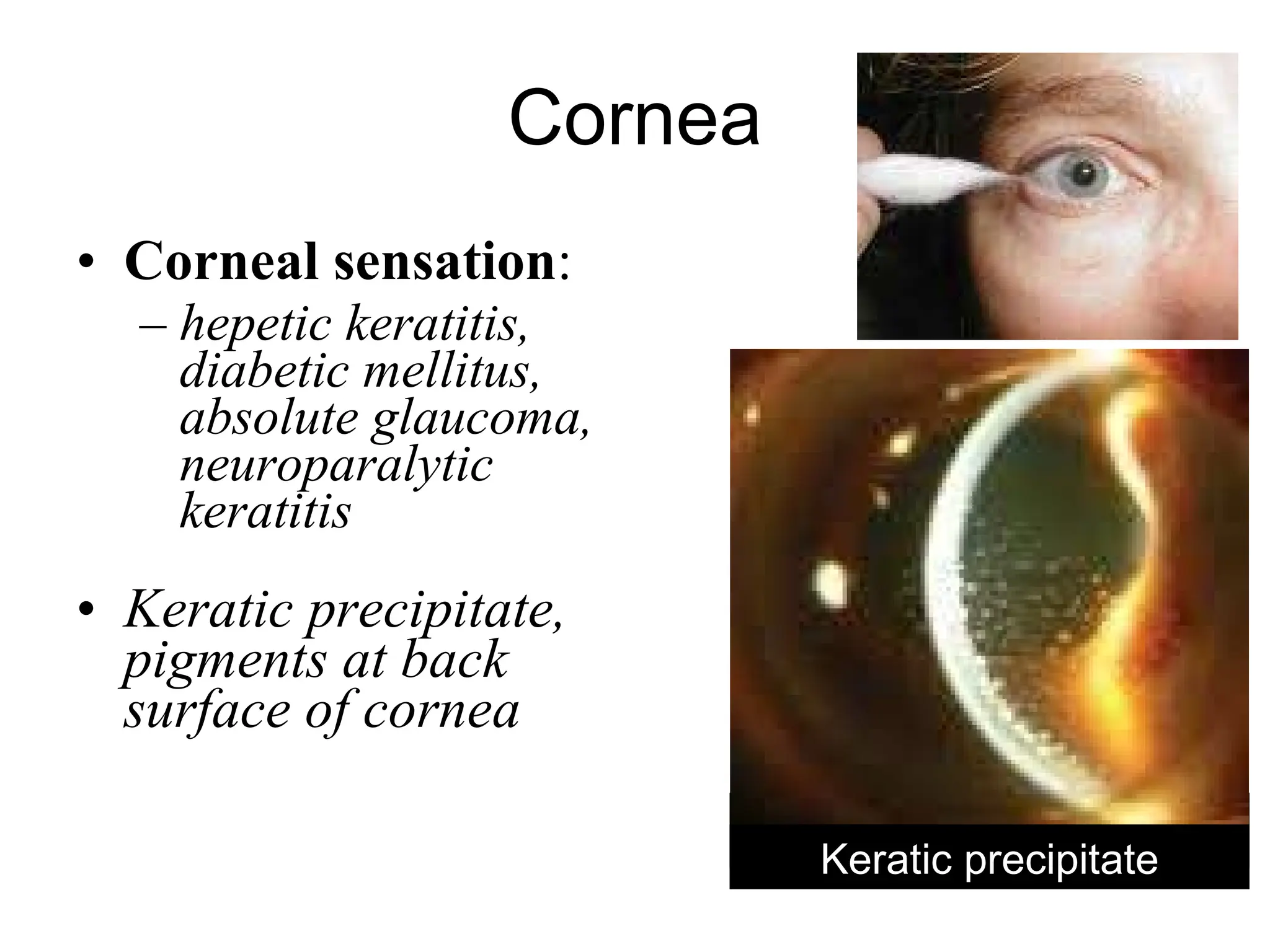
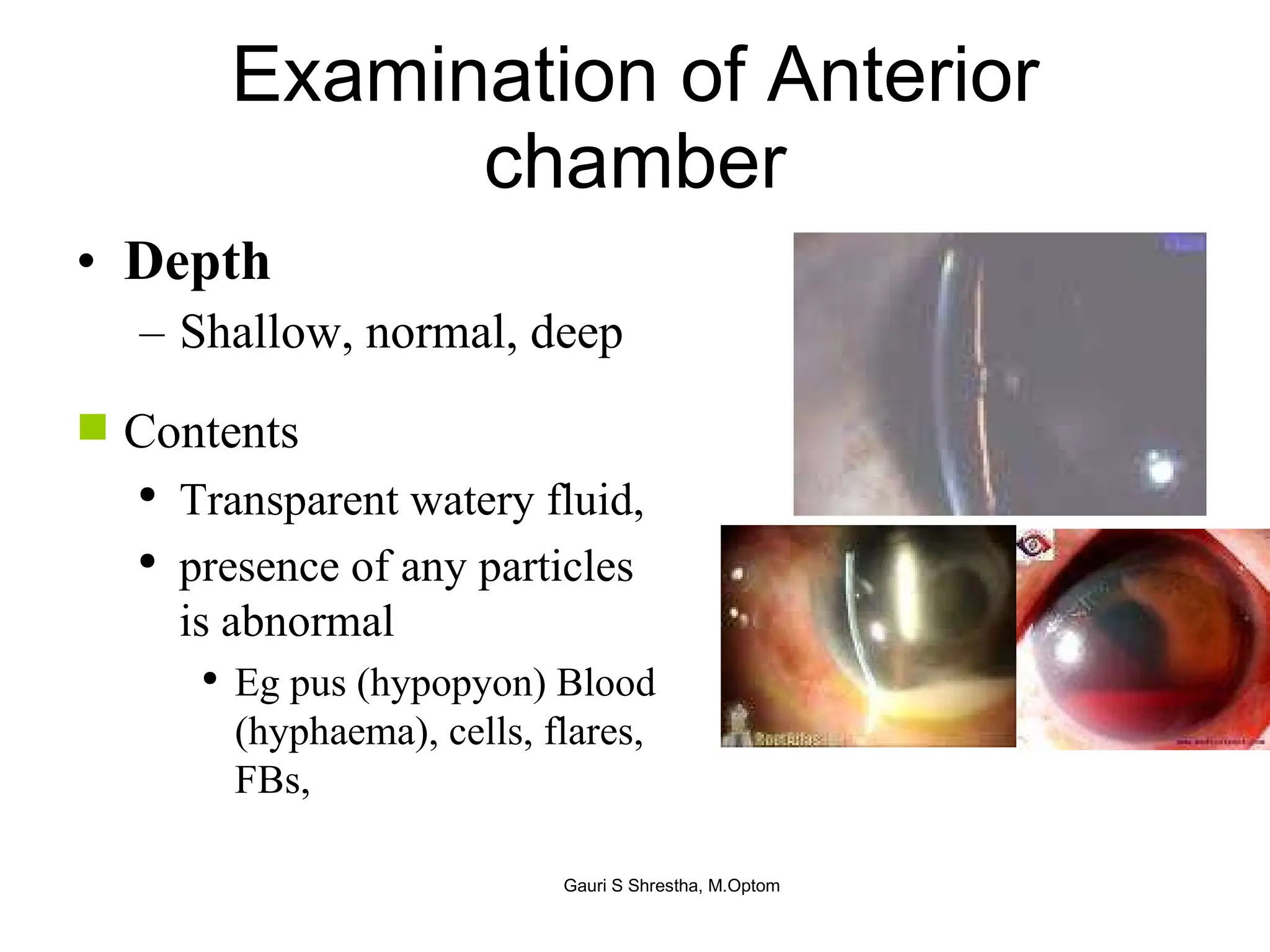
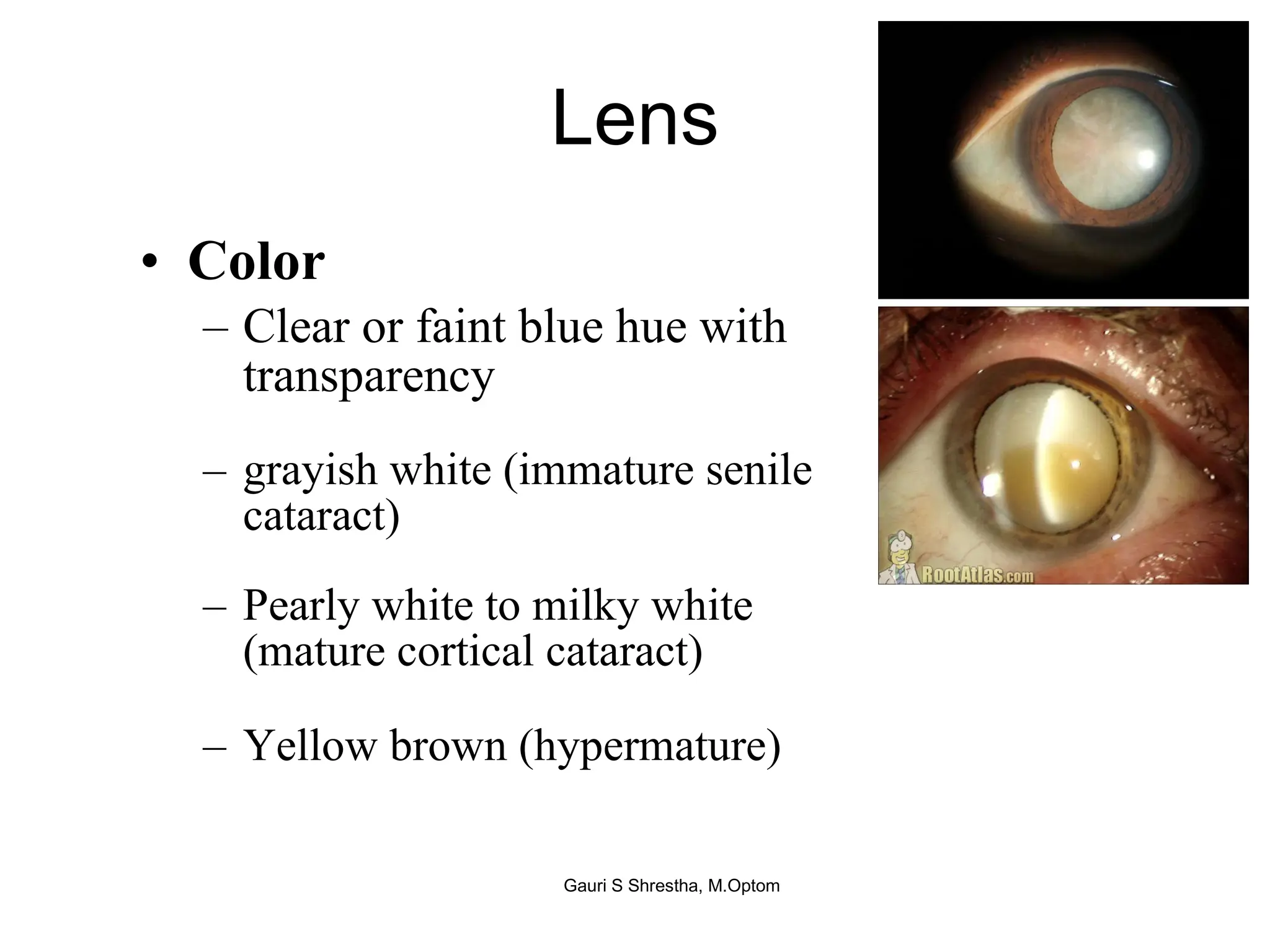
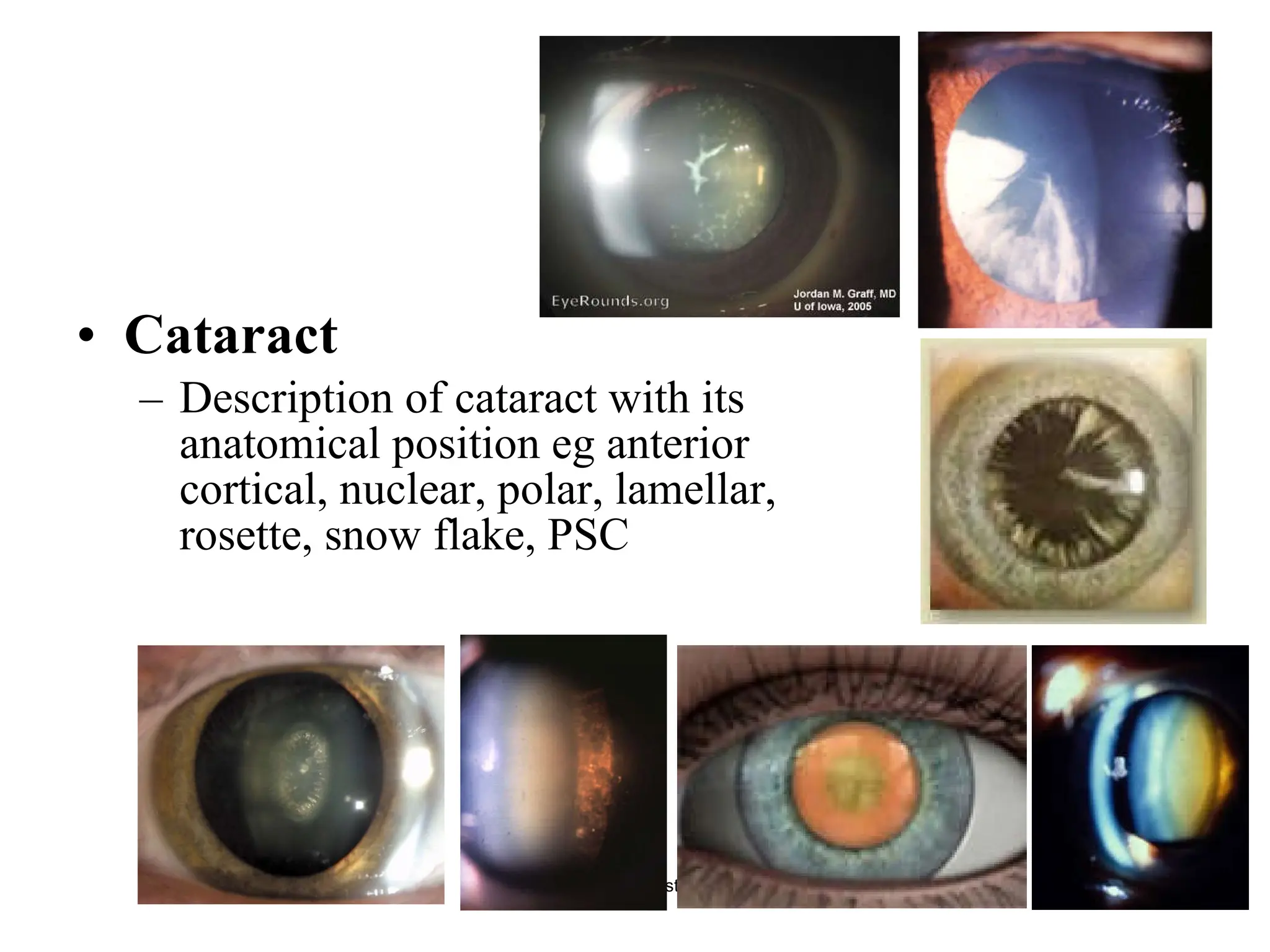
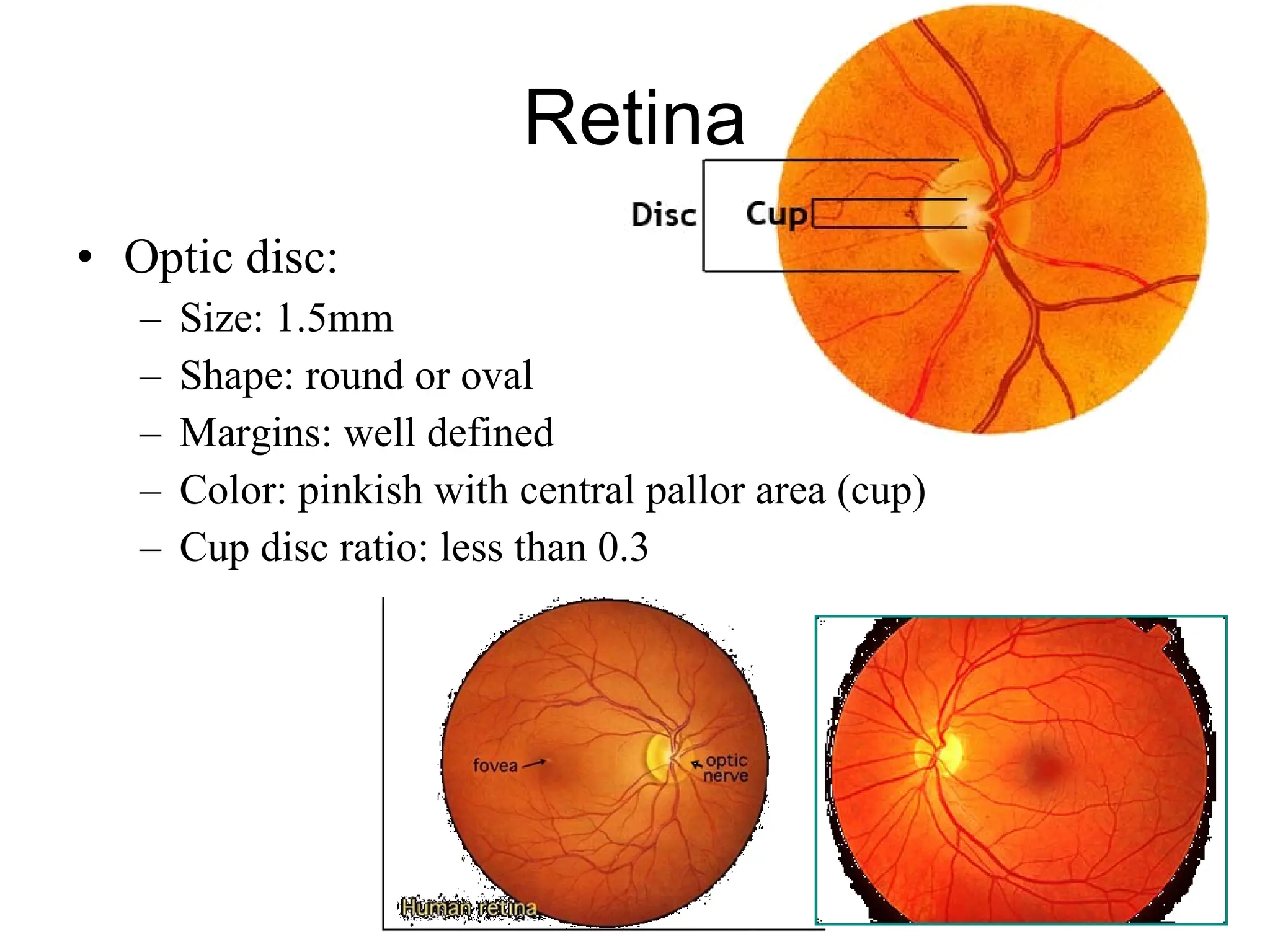
The document outlines a comprehensive nursing assessment of the eye, detailing the importance of patient history, visual acuity testing, eye alignment tests, and examinations of various eye structures. It emphasizes the need for thorough patient preparation, accurate history-taking, and specific tests to ensure accurate diagnoses and management plans. Additionally, it discusses tools and methods for assessing various ocular conditions, illustrating the significance of eye health in nursing care.