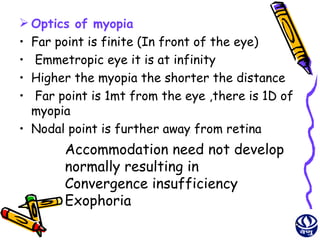
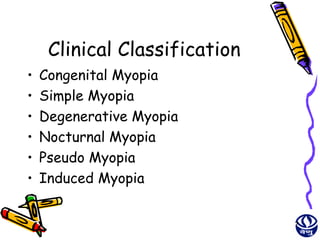
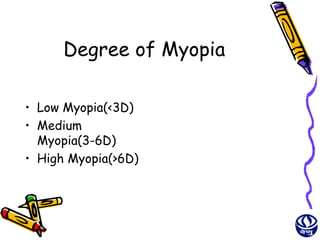
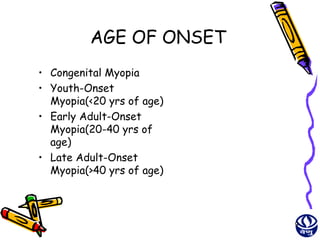
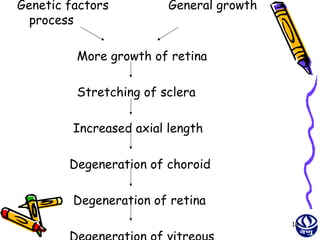
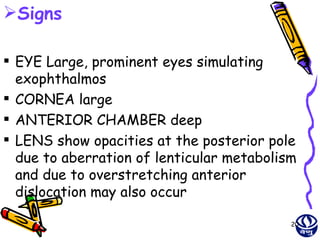
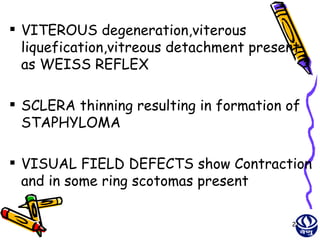
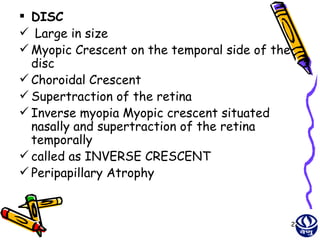
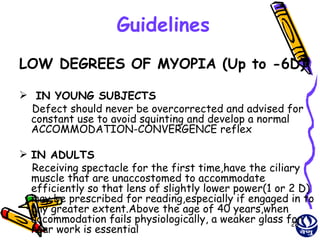
This document provides information about myopia (nearsightedness), including its definition, causes, types, classifications, signs and symptoms, and treatment options. It discusses the different mechanisms that can cause myopia, including excessive axial length growth. It classifies myopia based on clinical features, degree, and age of onset. Treatment options covered include optical correction with glasses or contact lenses, as well as surgical procedures like LASIK, PRK, phakic IOL implantation, and corneal ring segments.



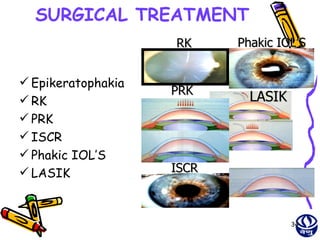
![Photorefractive
Keratectomy
(PRK)
• Involves direct laser ablation of corneal
stroma after removal of corneal epithelium
mechanically or using a laser beam.
• Done using Excimer laser
• MUNNERLYN EQN: depth of ablation
(micrometer)=[diameter of optical
zone(mm)]² × 1/3power(Diopter)
• For myopic a large amount of ablation is
done in central cornea than in the
periphery.
• Give good results for -2D to -6D of myopia 35](https://image.slidesharecdn.com/myopia-120612033316-phpapp01/85/Myopia-35-320.jpg)