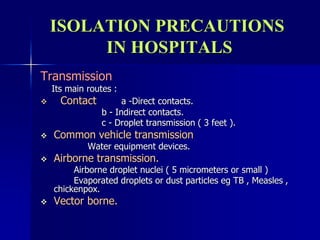
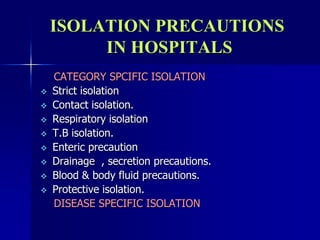
This document discusses isolation precautions in hospitals. It outlines the rationale for isolation precautions, noting that infection transmission requires a microorganism, source, susceptible host, and means of transmission. Various sources of infection and host factors are described. The main routes of transmission - contact, droplet, airborne, and vector-borne - are explained. Guidelines for isolation precautions from the CDC in 1983, 1990, and 1996 are summarized. These include category-specific and disease-specific isolation as well as standard and transmission-based precautions. Specific precautions for airborne, droplet, and contact transmission are provided. Fundamental aspects of isolation precautions like hand washing, gloves, patient placement, and transport are also covered