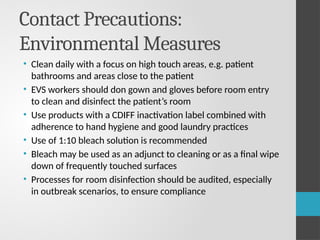
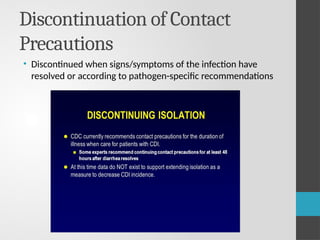
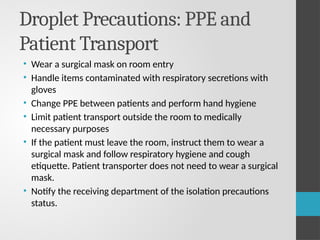
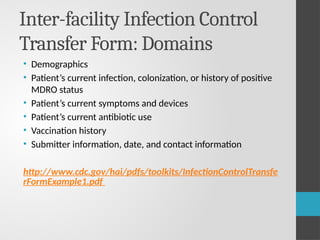
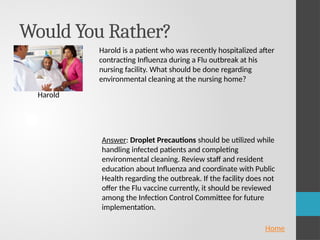
This document is a workshop presentation focusing on transmission-based precautions for managing multidrug-resistant organisms (MDROs) in long-term care facilities. It outlines the definitions, types of transmission (contact, droplet, airborne), standard precautions, and specific guidelines for patient placement, personal protective equipment (PPE), and environmental cleaning. Emphasis is placed on the importance of education, adherence monitoring, and infection control strategies to prevent the spread of infections within healthcare settings.