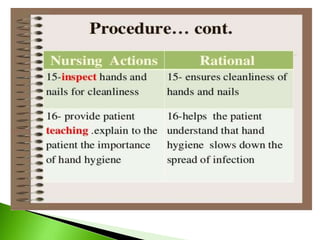
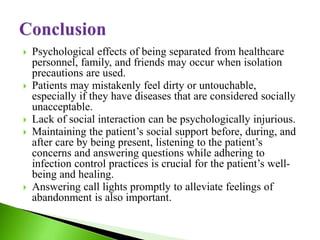
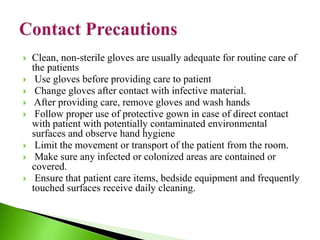
The document discusses isolation precautions and barrier nursing techniques used to prevent the spread of infection in clinical settings. It defines isolation as techniques used to limit the spread of infection from infected to non-infected individuals. Barrier nursing refers to stringent infection control techniques used in nursing to protect medical staff and isolate infectious patients. The document outlines various isolation precautions like contact, airborne and droplet precautions. It emphasizes the importance of proper use of personal protective equipment, hand hygiene, environmental cleaning and other standard safety precautions to interrupt transmission of microorganisms in healthcare settings.
![UNIT XI INFECTION CONTROL IN CLINICL SETTING
TOPIC:ISOLATION PRECAUTIONS [ BARRIER NURSING ]
Presented By:
Mrs Bemina JA
Assistant Professor
ESIC College of Nursing
Kalaburagi](https://image.slidesharecdn.com/barriernsg-220903064431-b2fe2b74/85/barrier-nsg-pptx-1-320.jpg)






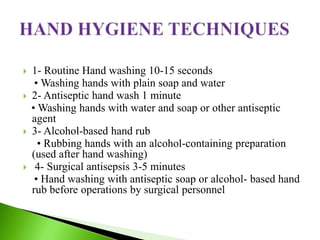
![ 1. Aseptic technique[Hand Washing]
2. Isolation
3.Personal protective equipments
4. Decontamination of equipments and unit[Safer Handling
of Sharps, Linen handling and disposal]
5. Waste disposal
6. Transportation of infected patients [Handling Biological
Spills
7. Standard safety precautions[Universal precautions]
7. Environmental cleaning
8. Risk assessment
9. Staff health](https://image.slidesharecdn.com/barriernsg-220903064431-b2fe2b74/85/barrier-nsg-pptx-11-320.jpg)