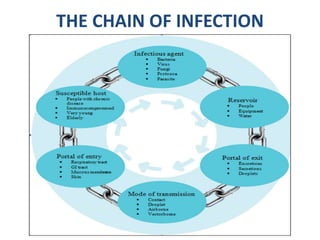
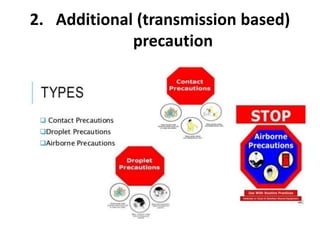
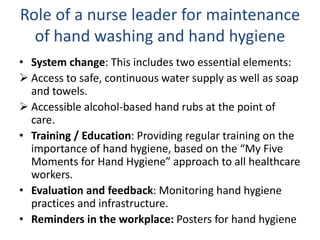
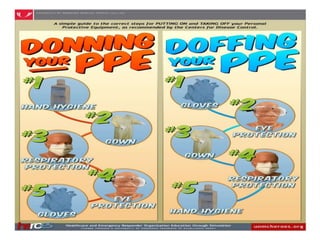
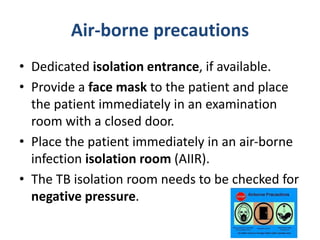
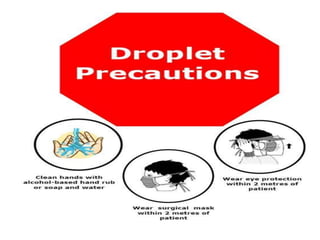
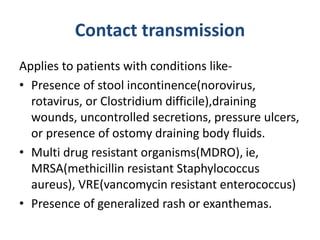
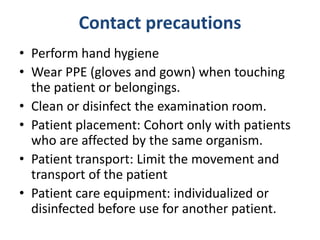
An infection control program aims to restrict the spread of infections in healthcare facilities through applying research-based practices. The key components of an infection control program include standard and transmission-based precautions, healthcare worker education and protection, risk minimization, and surveillance. Standard precautions like hand hygiene and personal protective equipment are applied to all patients, while additional airborne, droplet, and contact precautions depend on the specific infection's transmission mode. Proper implementation of infection control measures can reduce patient and staff infections.