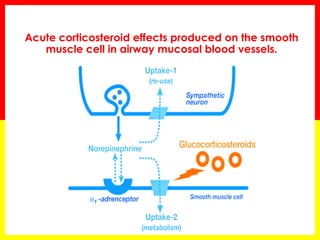
1. Inhaled corticosteroids (ICS) have both genomic and non-genomic mechanisms of action in acute asthma. The genomic effects occur slowly over hours through gene transcription, while the non-genomic effects occur rapidly within minutes through membrane receptor pathways.
2. The non-genomic effects of ICS include reducing airway blood flow through vasoconstriction by enhancing norepinephrine action in smooth muscle cells. This leads to rapid improvements in spirometry and symptoms.
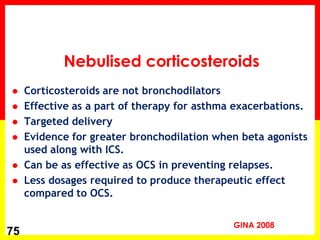
3. Multiple high doses of ICS administered frequently over 1-2 hours results in early clinical benefits, regardless of initial severity. ICS can be as effective as oral steroids for acute asthma exacerbations and