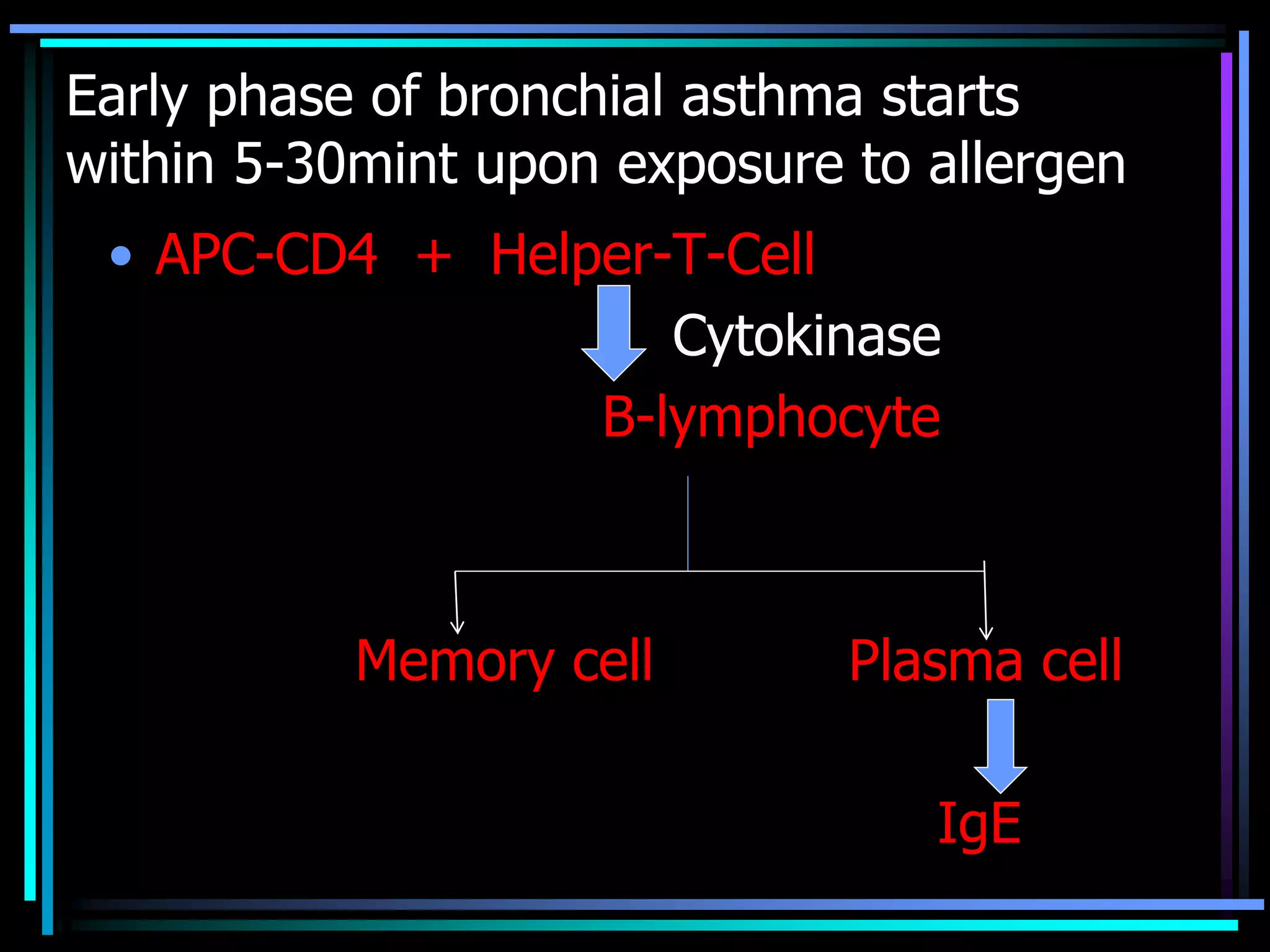
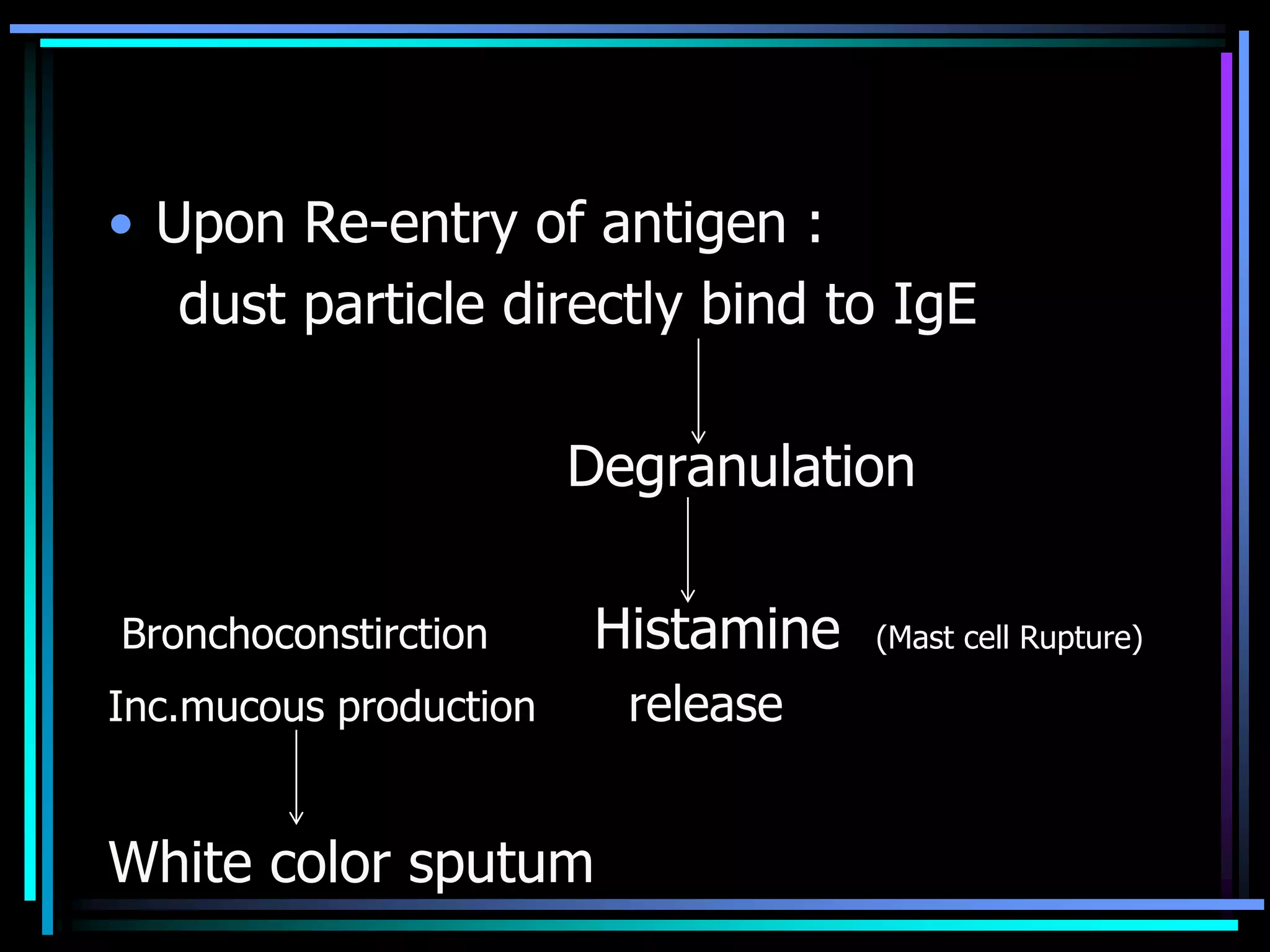
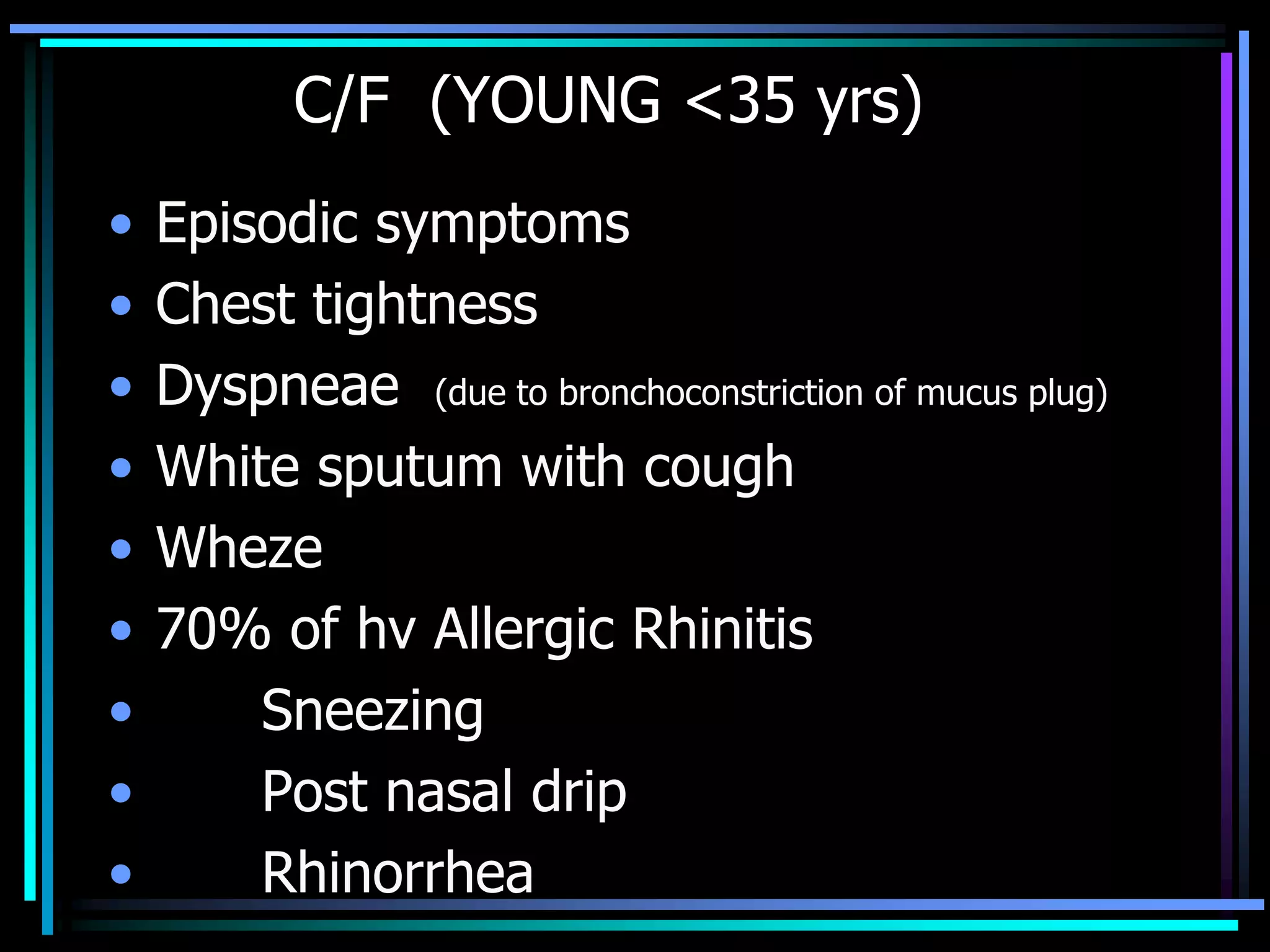
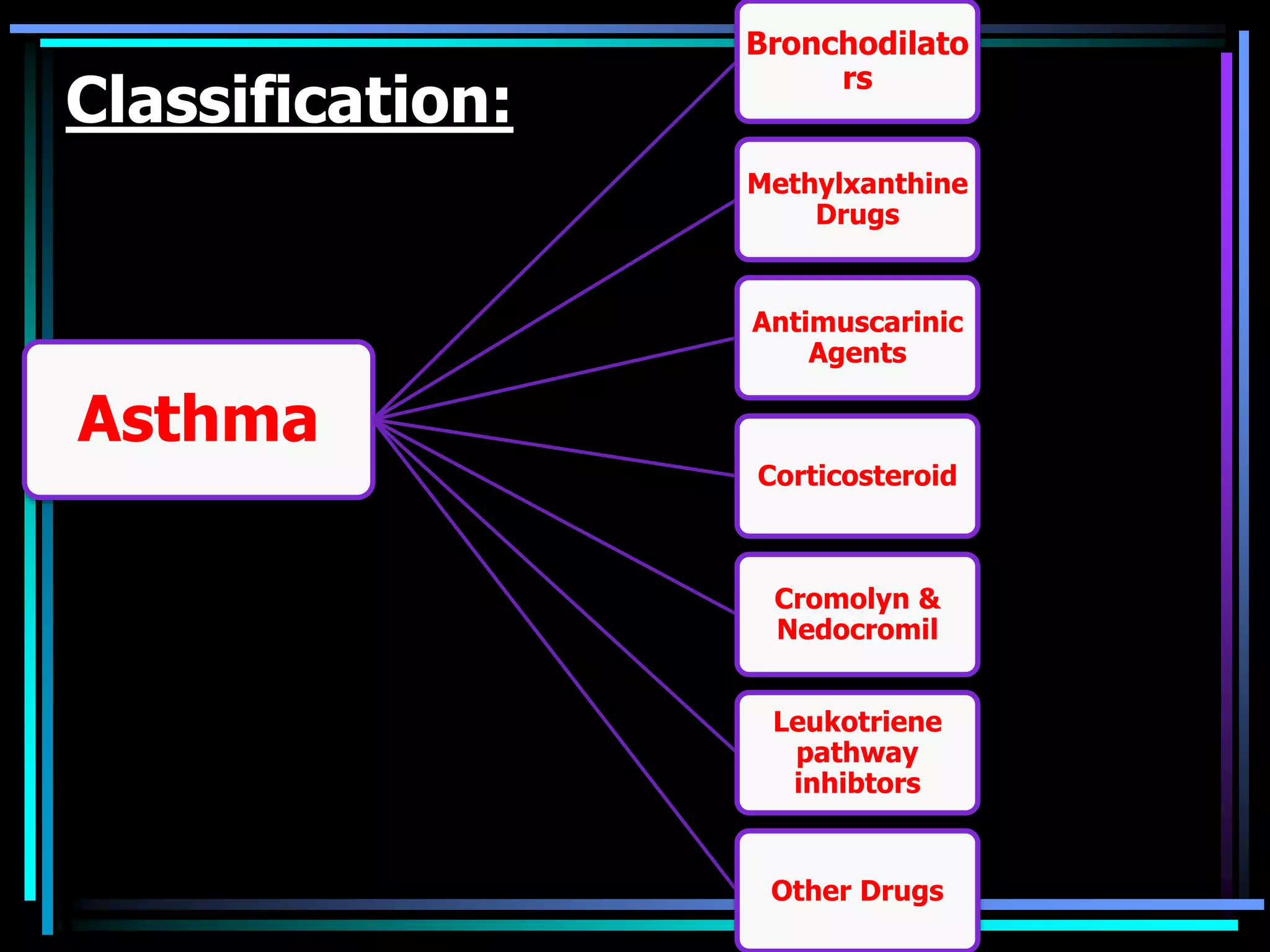
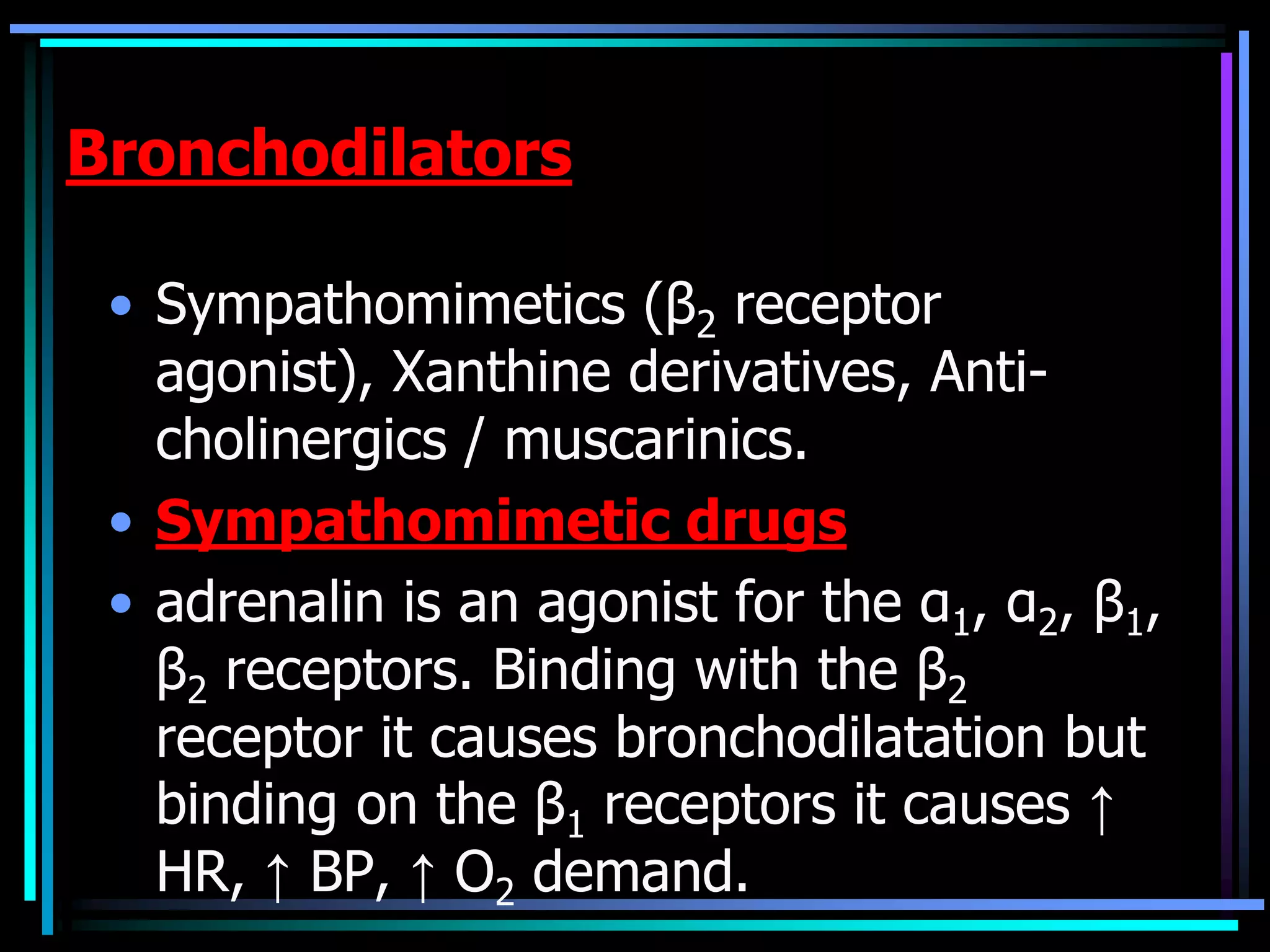
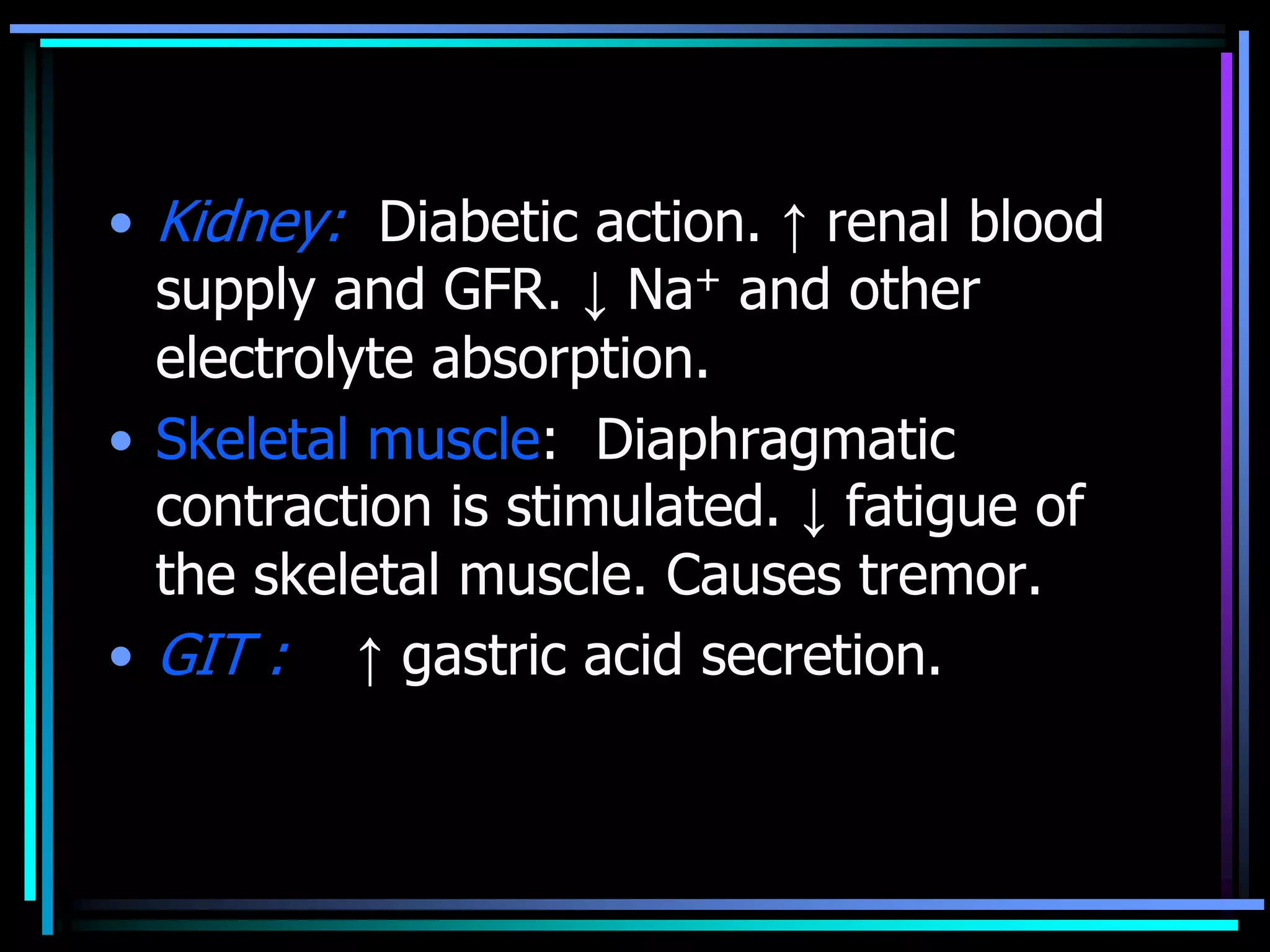
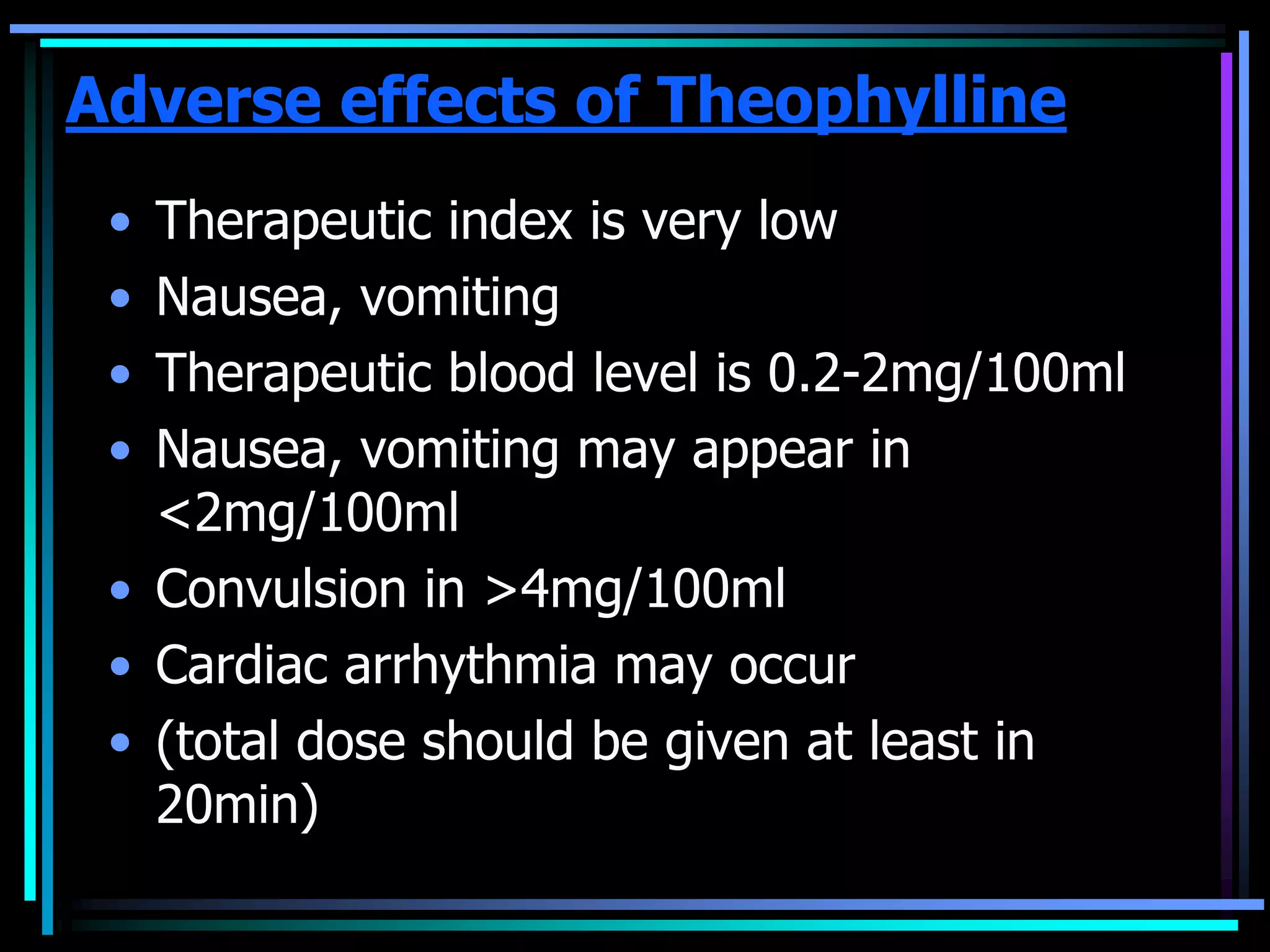
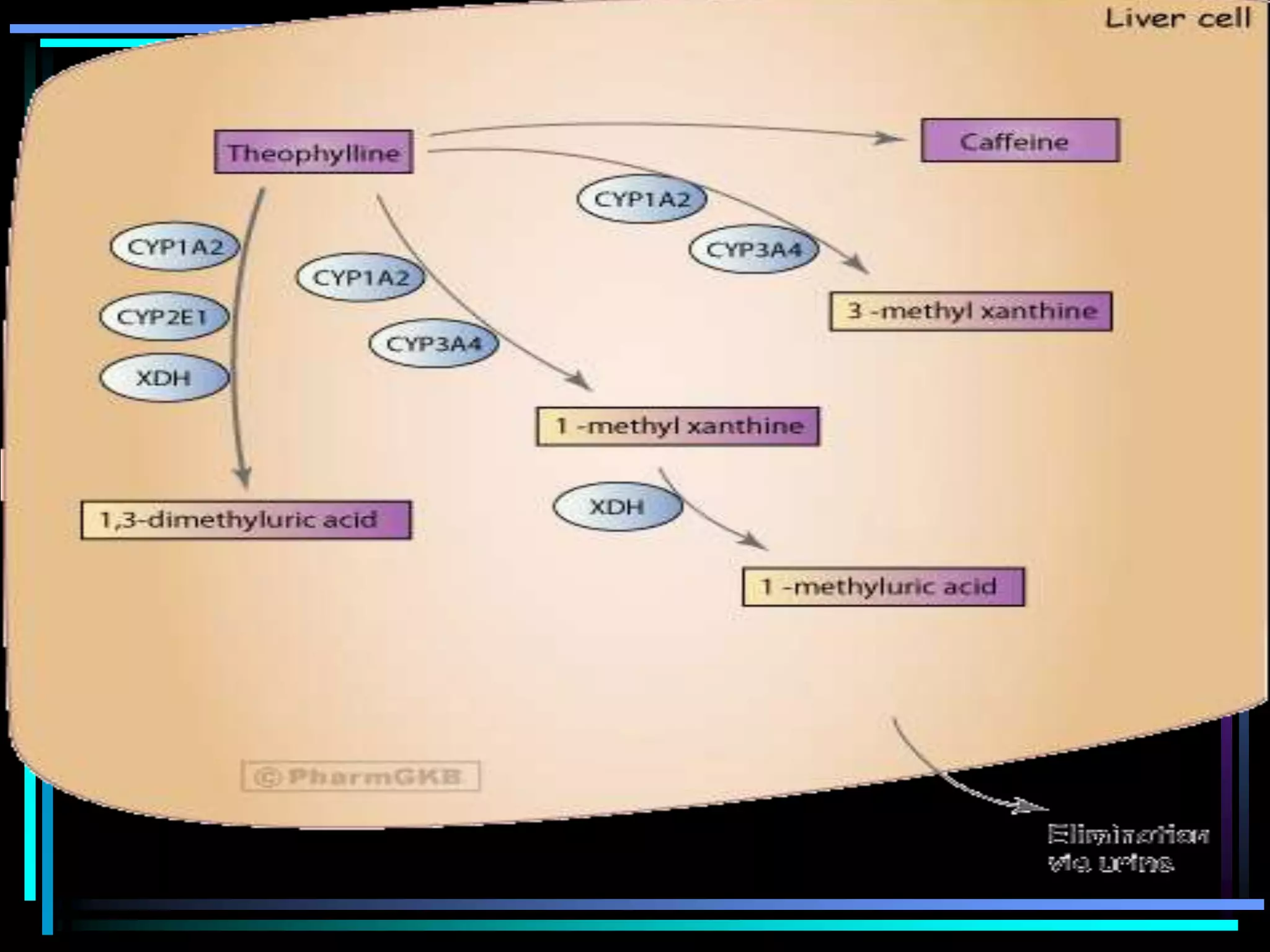
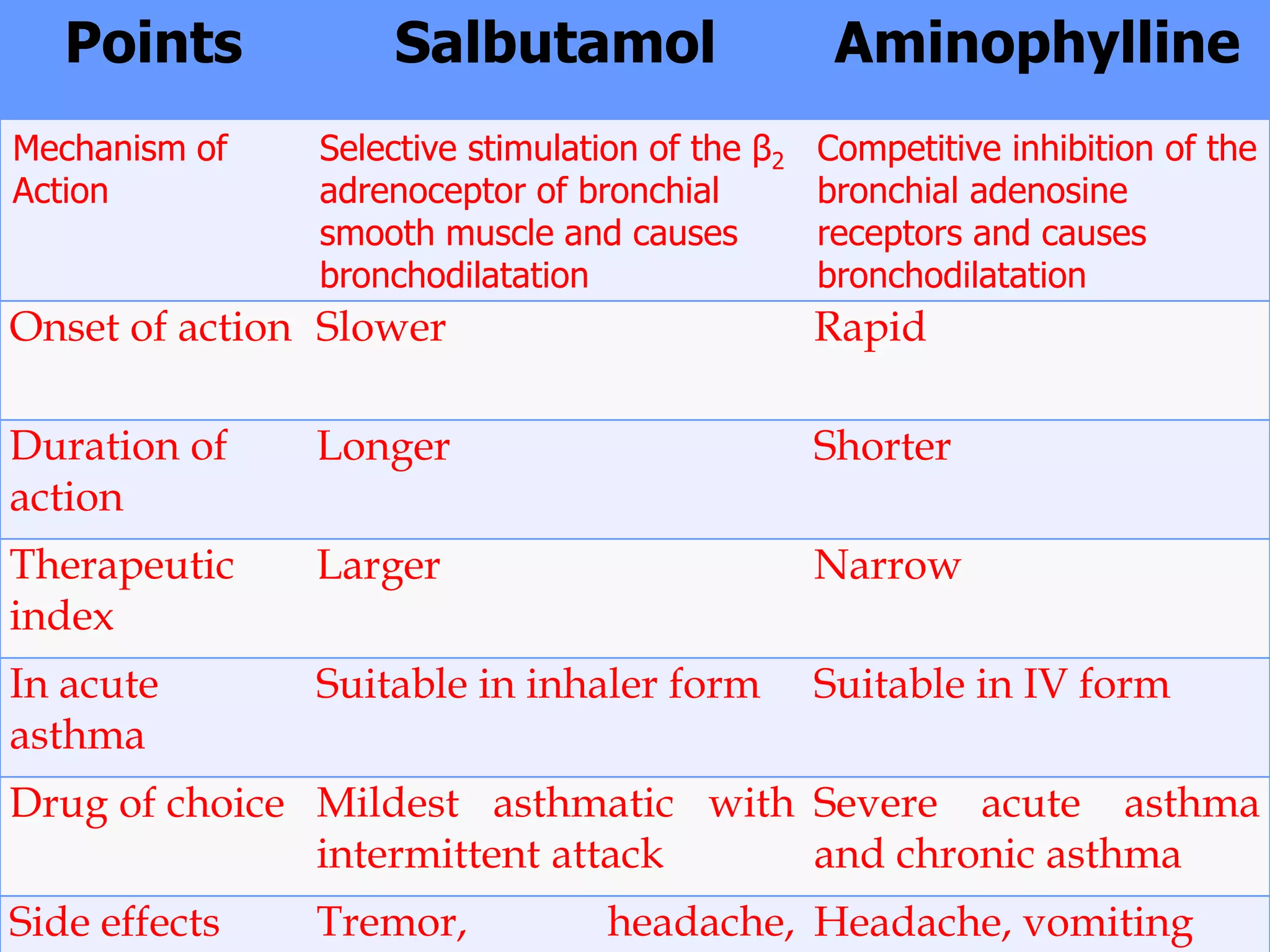
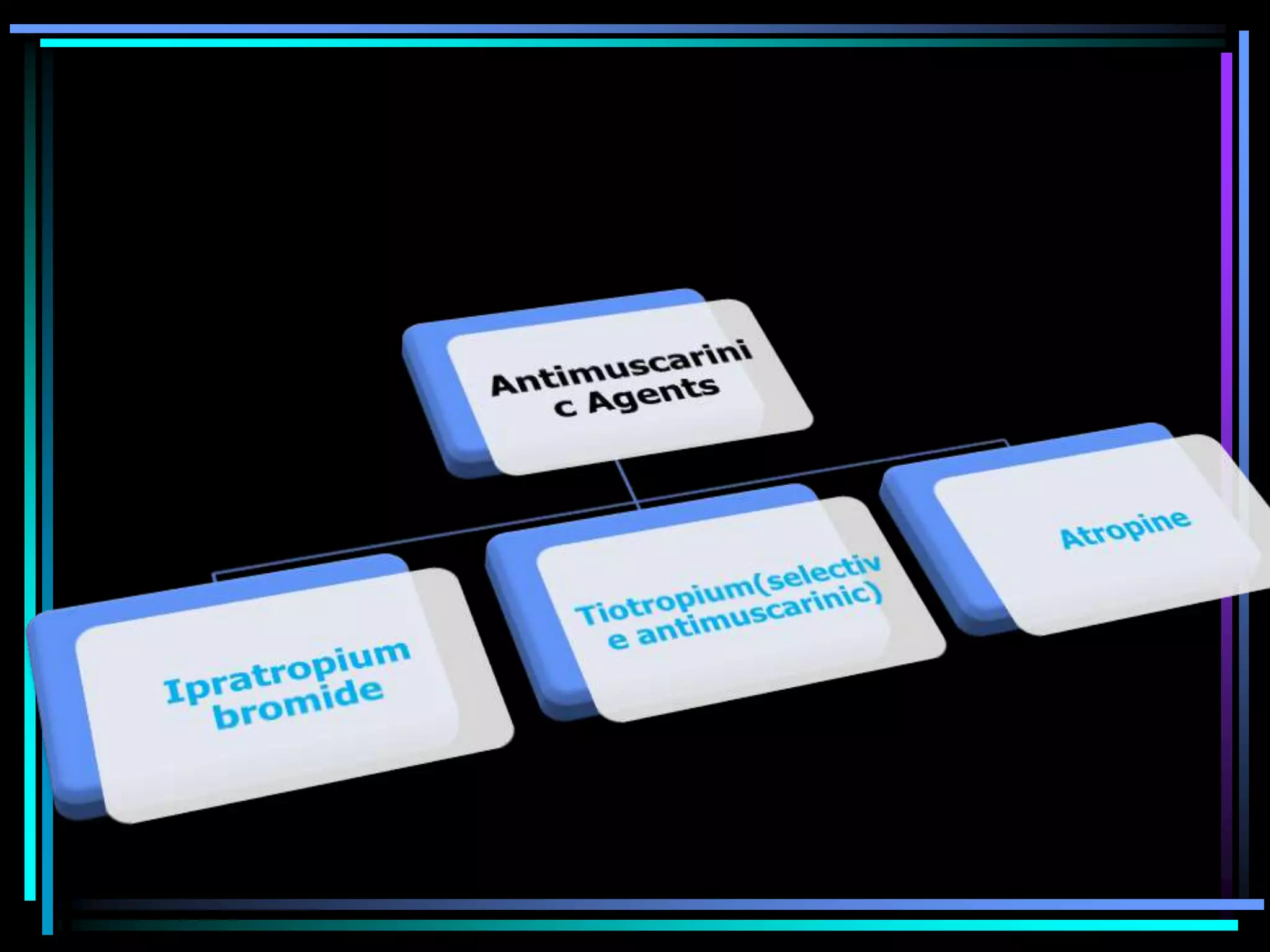
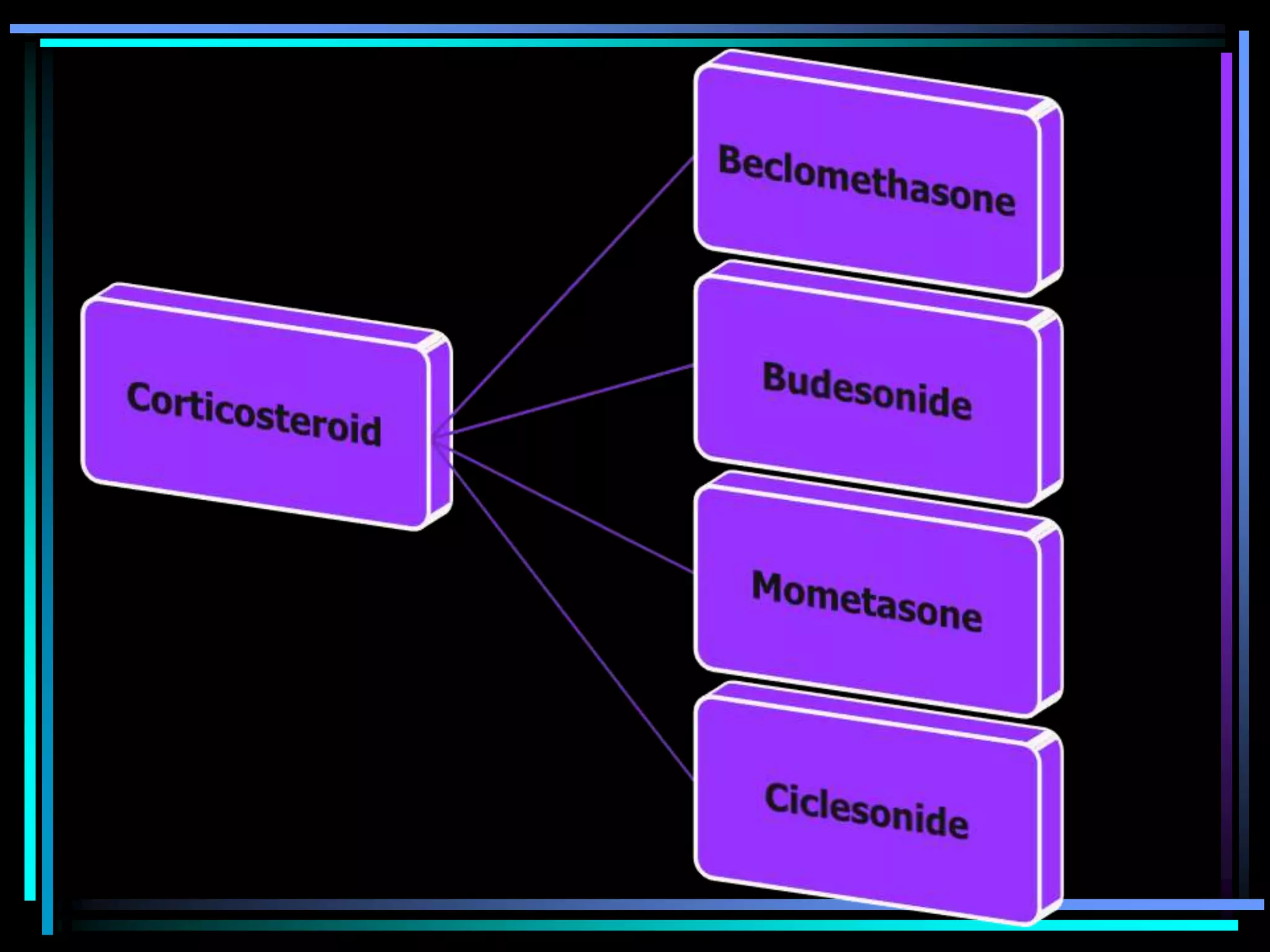
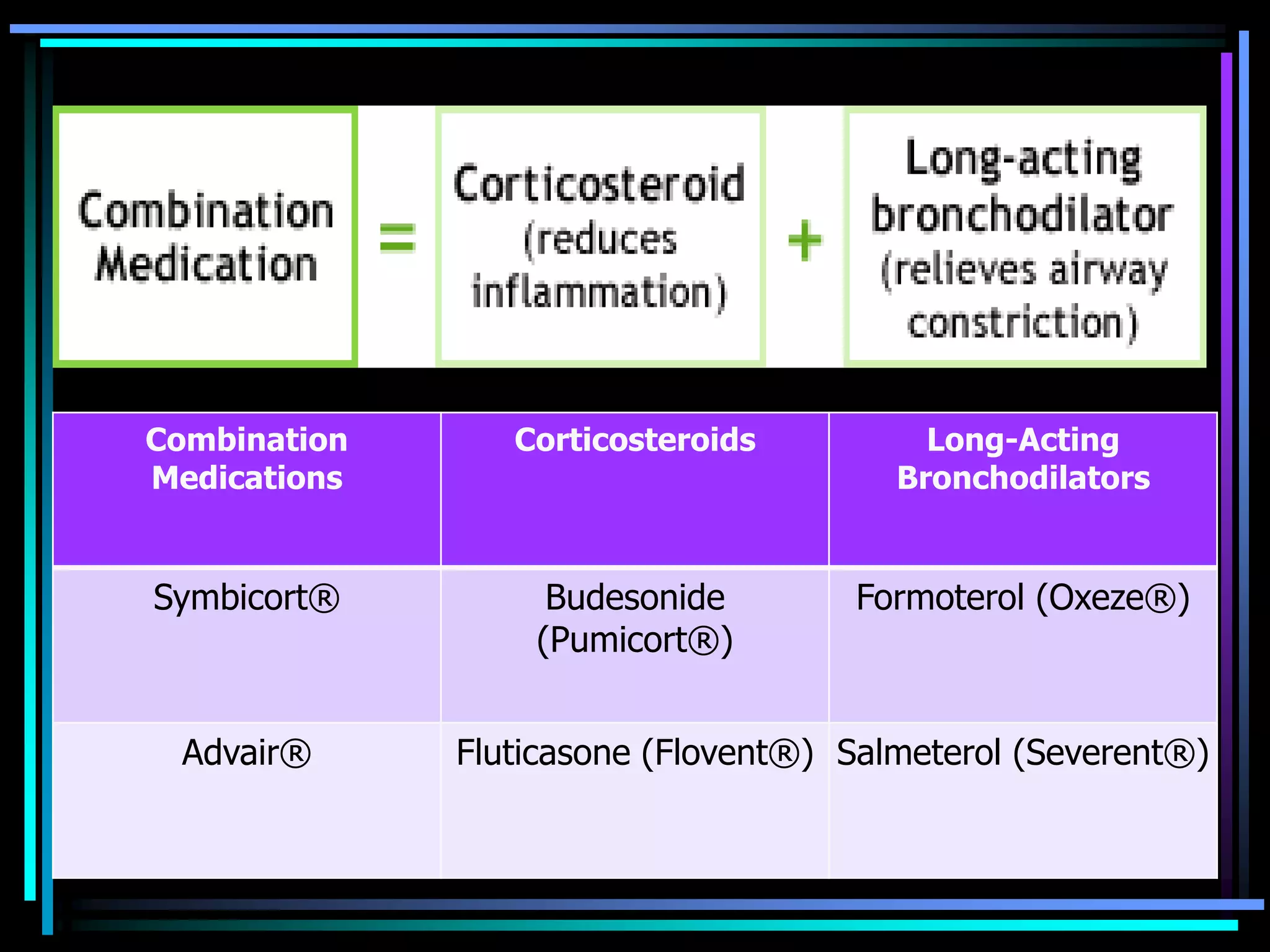
This document discusses asthma, including its causes, pathophysiology, classification, approach to treatment, and various medication options. It begins by defining asthma as a reversible condition of bronchial constriction in response to stimuli. Various medication classes are then summarized, including bronchodilators, corticosteroids, leukotriene inhibitors, and combination therapies. Side effects of the different medications are also briefly outlined.