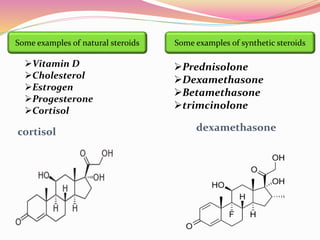
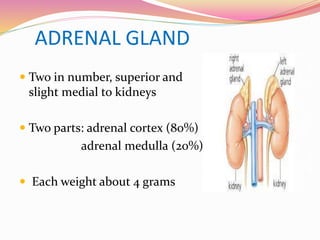
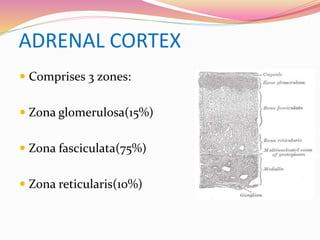
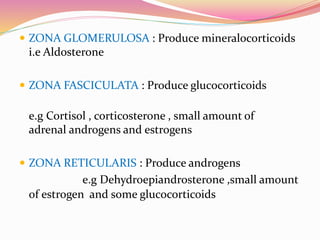
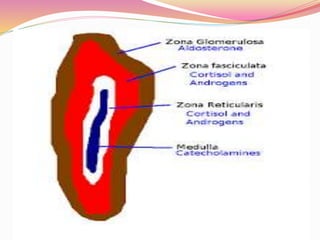
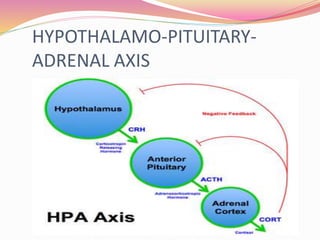
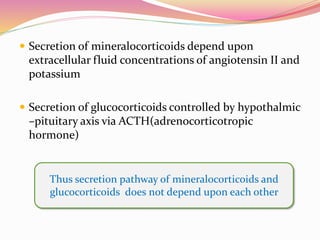
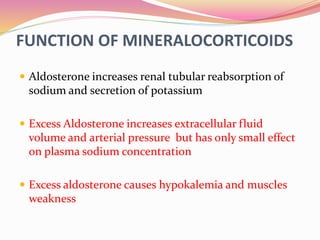
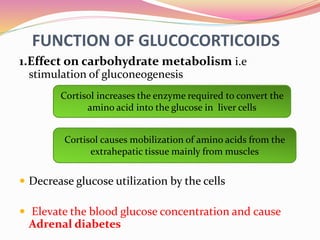
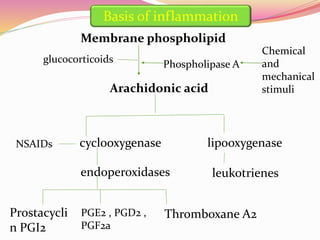
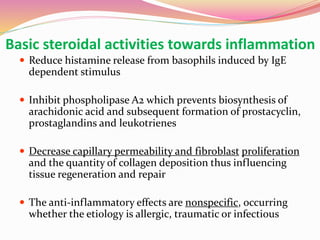
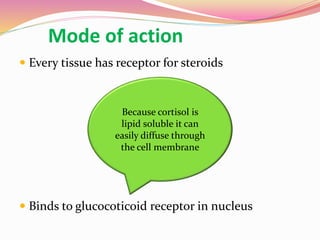
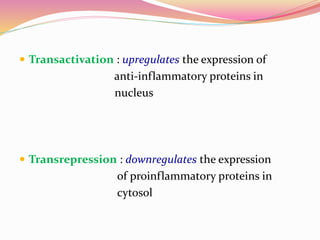
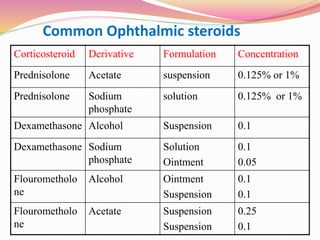
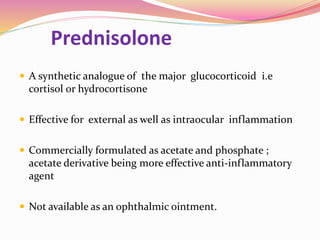
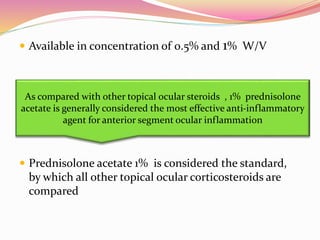
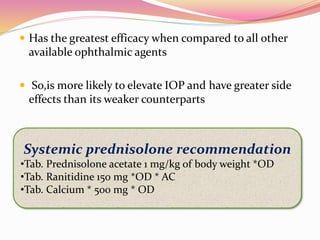
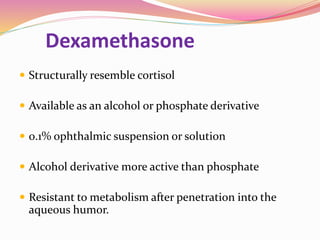
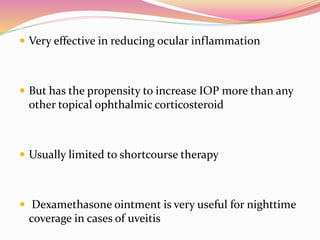
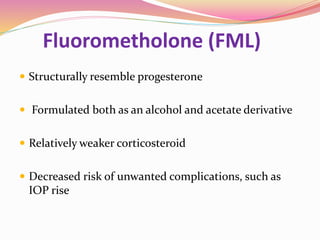
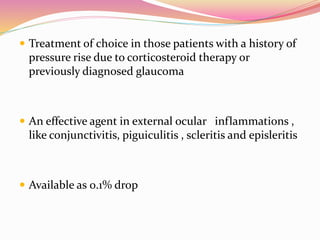
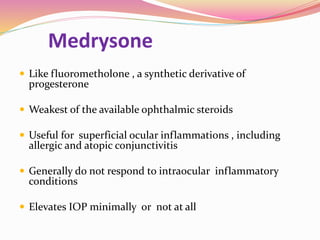
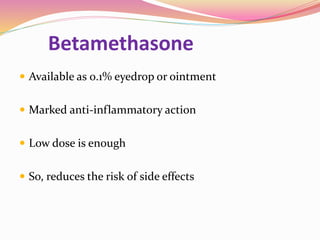
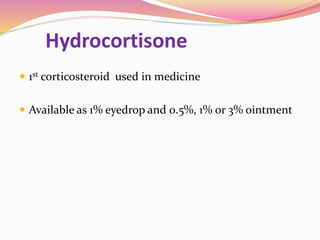
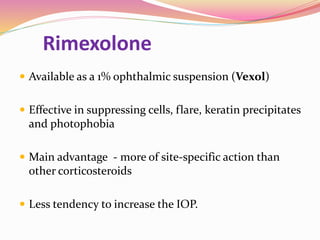
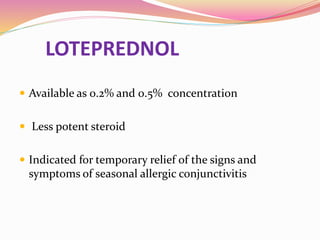
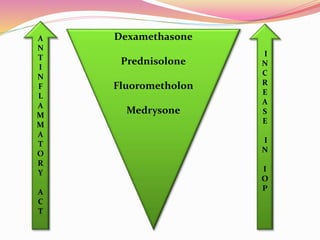
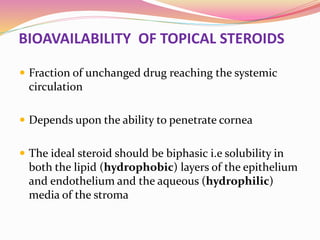
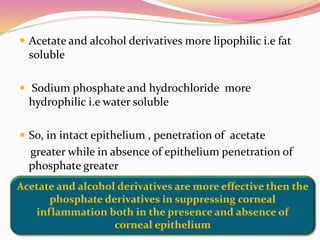
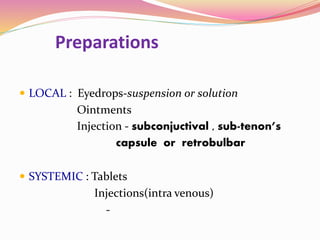
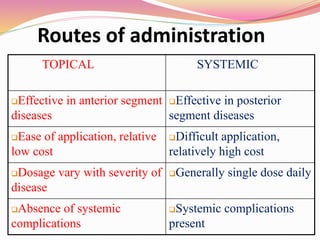
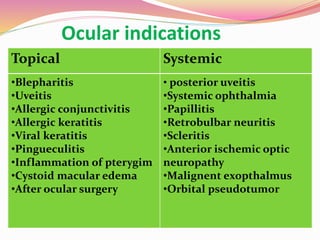
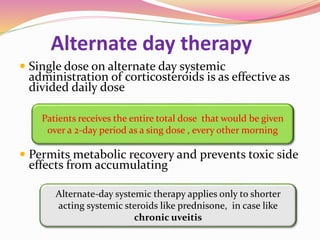
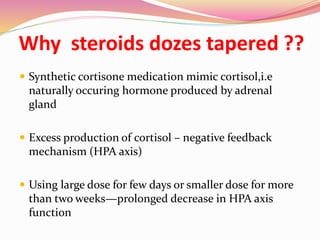
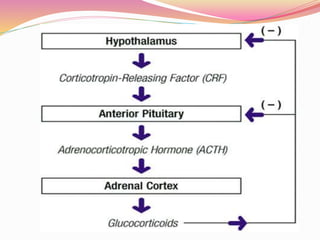
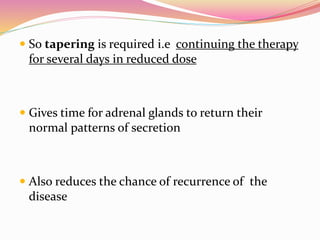
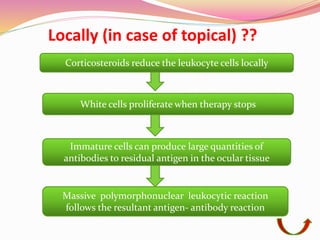
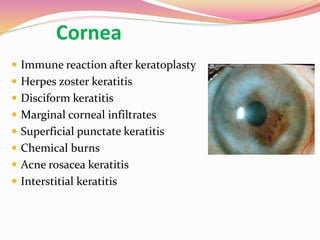
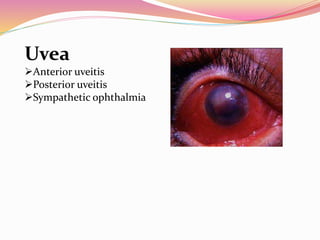
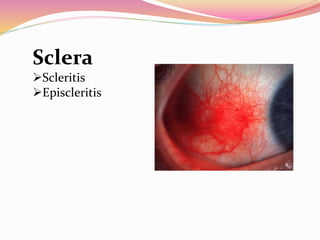
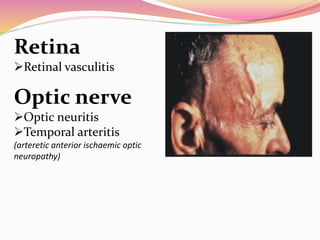
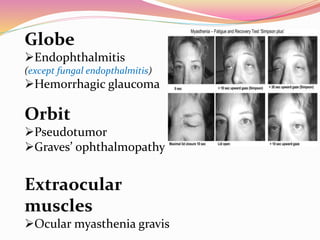
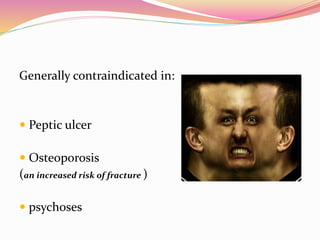
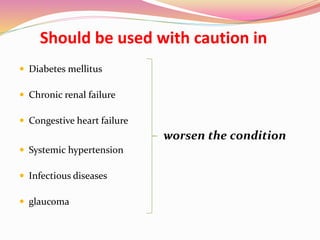
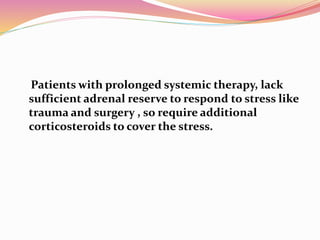
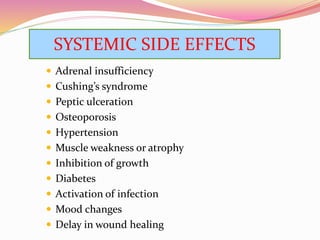
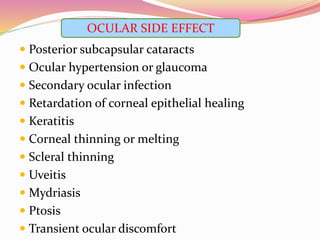
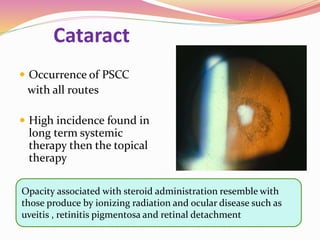
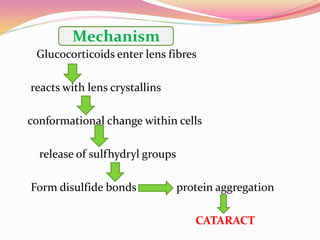
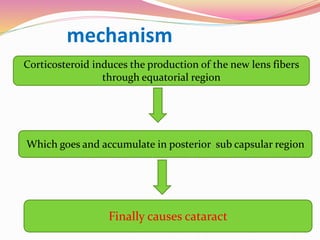
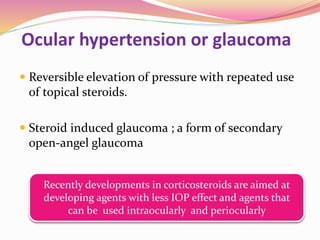
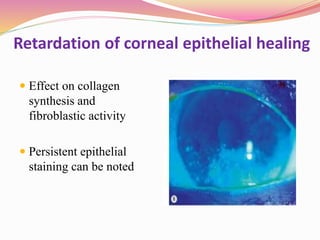
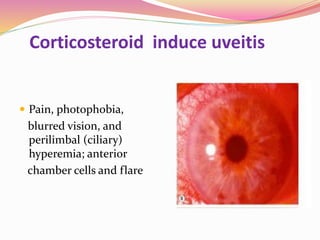
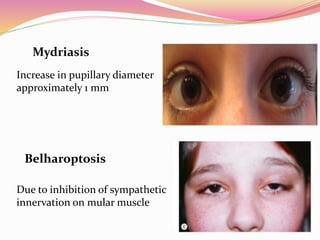
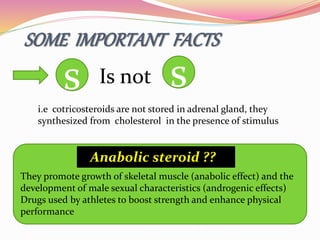
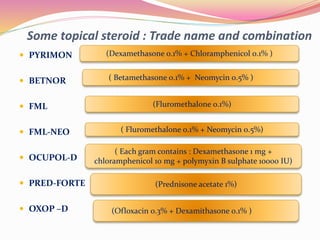
The document provides information about ocular steroids. It begins with an introduction to steroids and their chemical structure. It then discusses the adrenal gland and its role in producing steroids. The anti-inflammatory effects of steroids are explained through their impact on the inflammatory response pathway. Common ophthalmic steroids are listed along with their formulations and concentrations. The indications, contraindications and side effects of steroid use are briefly covered.