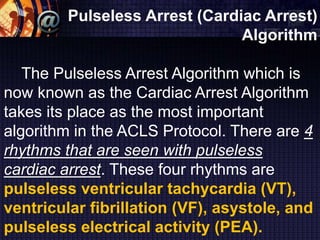
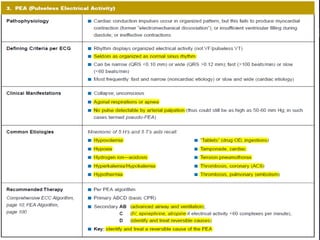
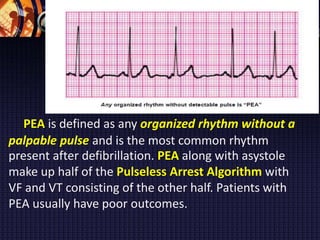
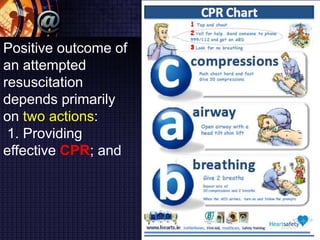
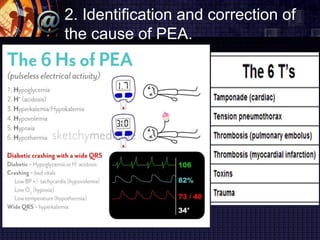
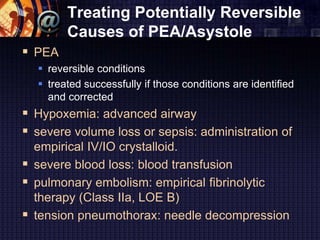
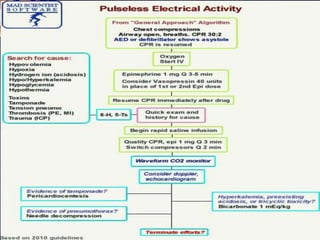
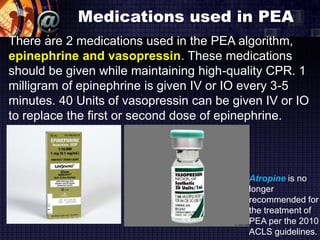
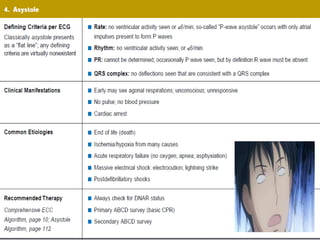
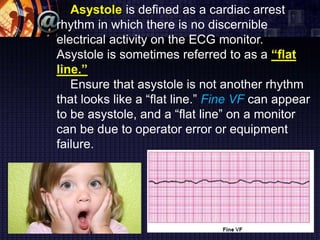
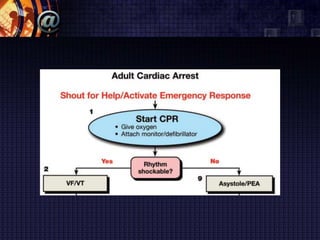
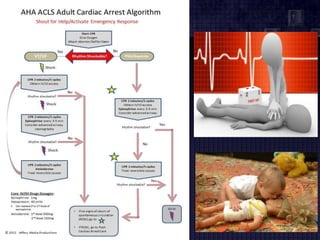
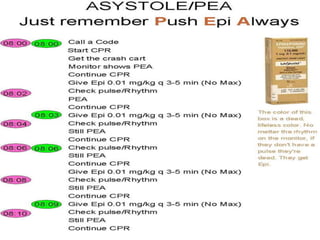
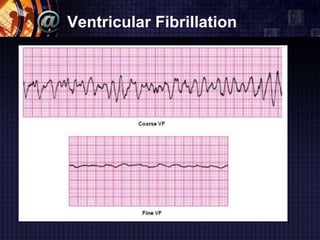
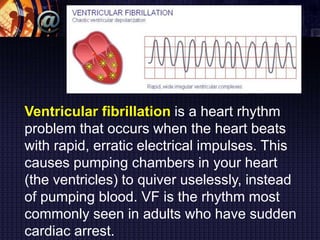
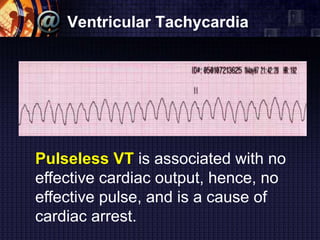
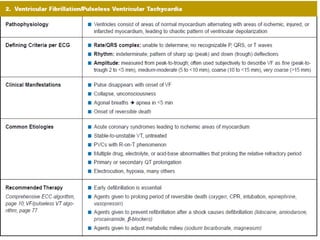
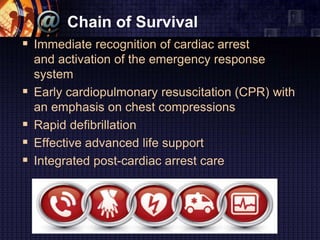
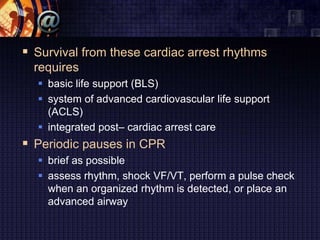
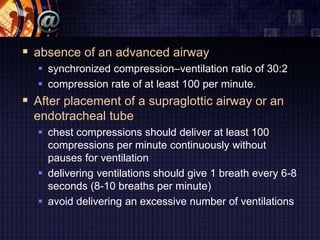
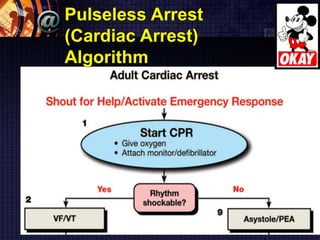
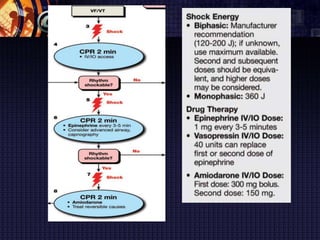
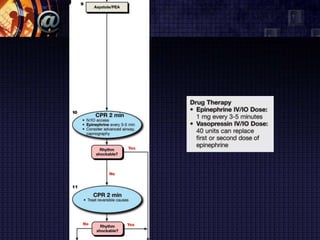
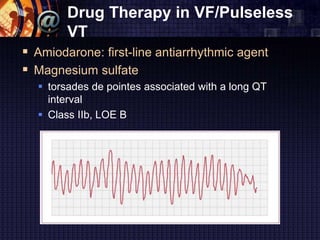
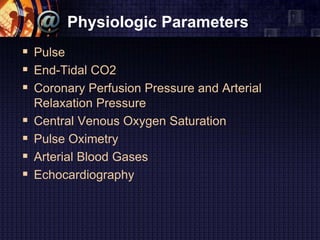
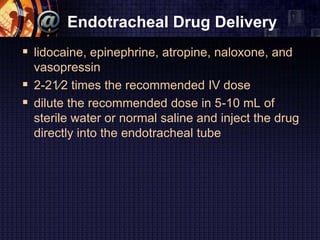
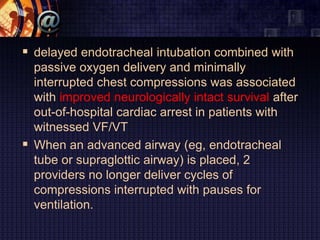
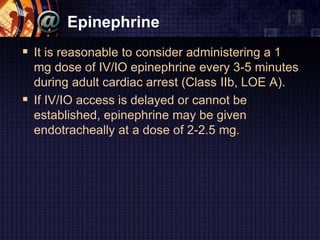
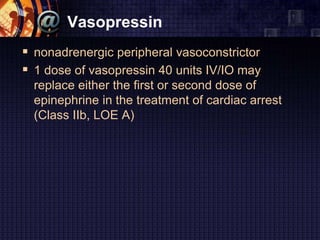
The document summarizes the pulseless arrest (cardiac arrest) algorithm. There are four rhythms seen with pulseless cardiac arrest: pulseless ventricular tachycardia, ventricular fibrillation, asystole, and pulseless electrical activity. PEA and asystole make up half of the algorithm and have poorer outcomes than VF and VT. Positive outcomes depend on high-quality CPR and identifying/treating the underlying cause. Epinephrine and vasopressin are used for PEA, while asystole is treated on the right side of the algorithm. VF is commonly seen in sudden cardiac arrest and is treated with defibrillation, while pulseless VT is also a cause of cardiac arrest