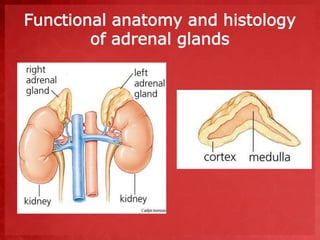
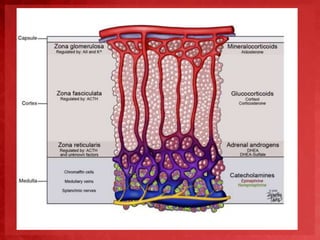
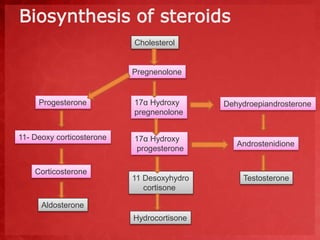
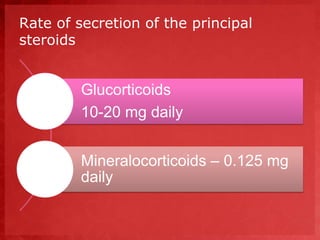
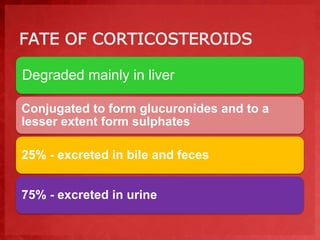
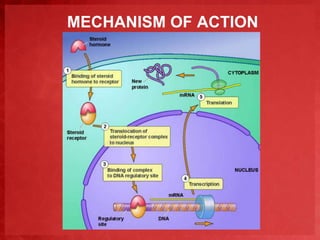
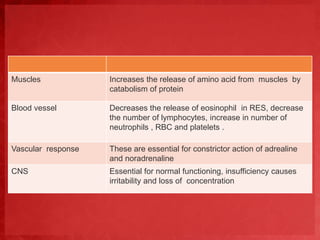
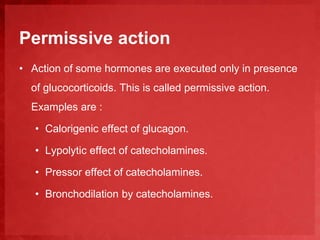
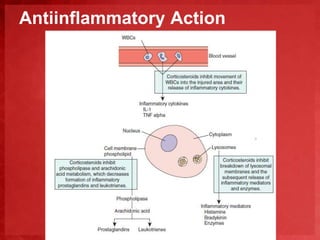
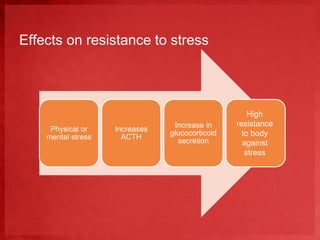
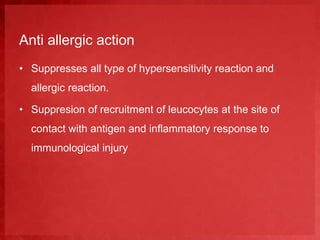
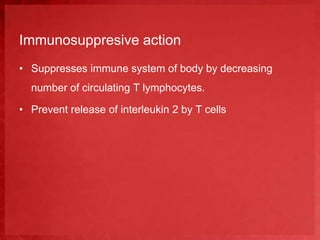
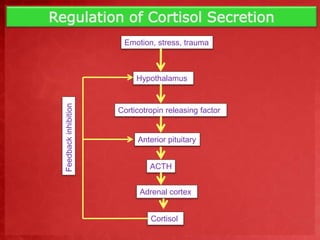
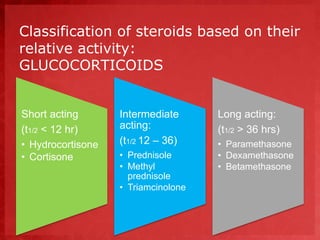
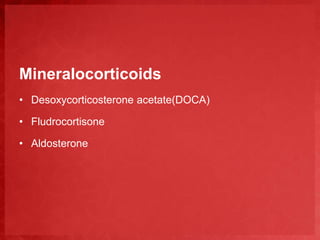
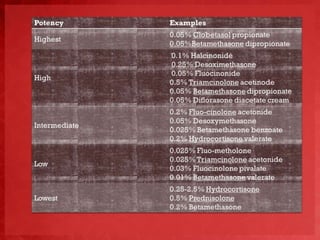
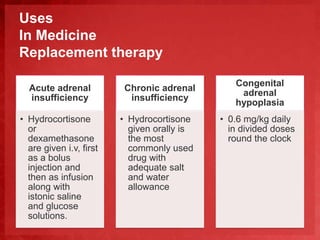
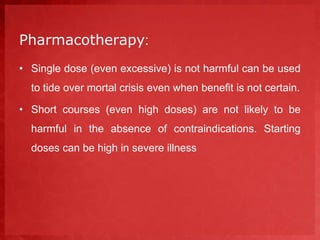
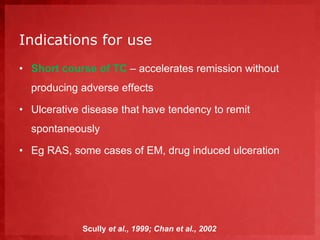
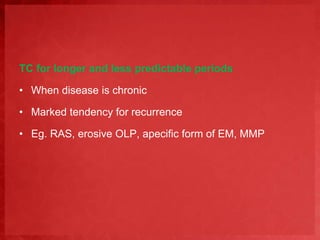
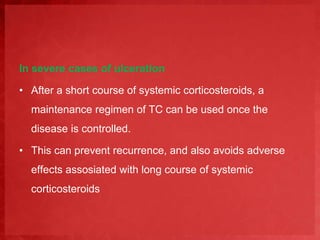
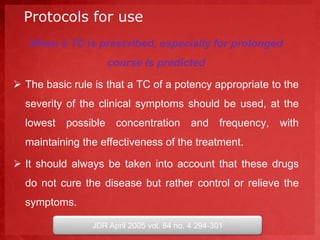
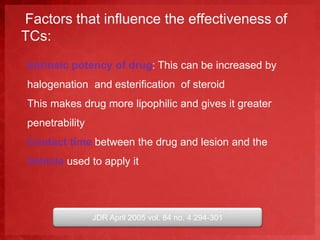
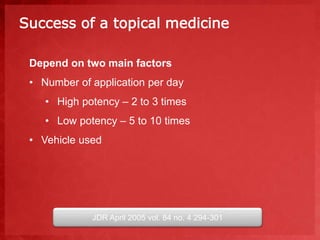
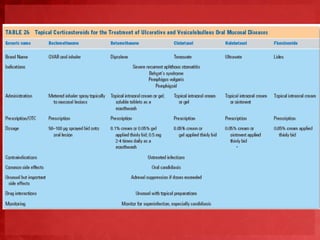
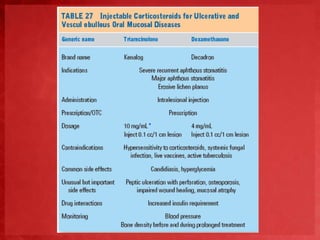
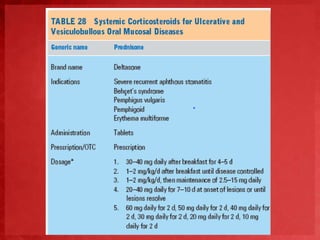
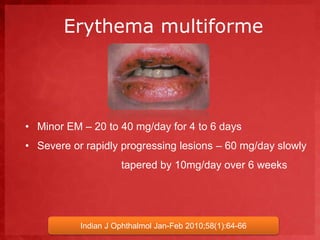
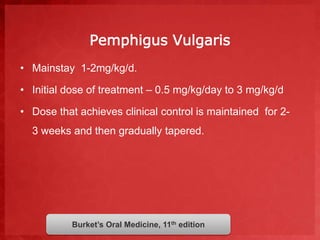
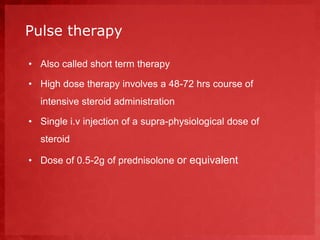
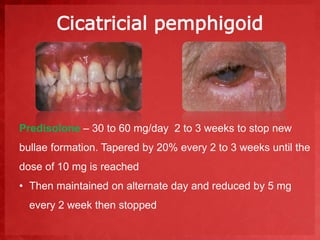
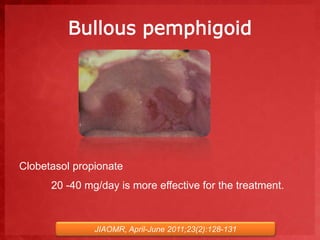
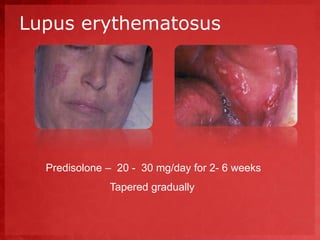
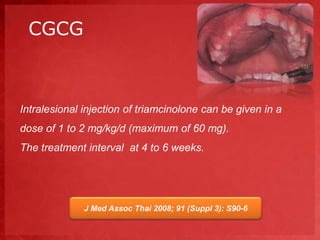
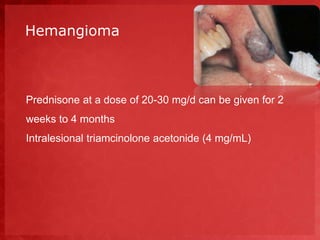
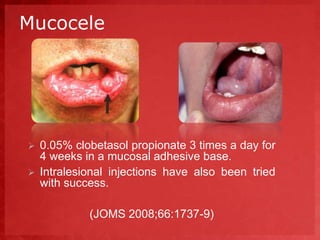
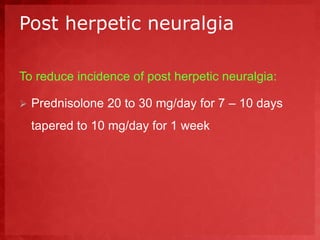
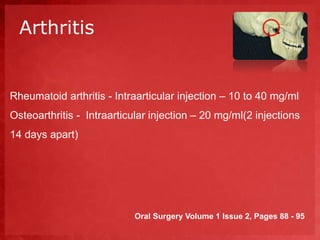
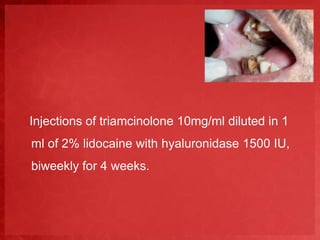
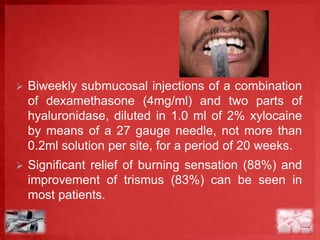
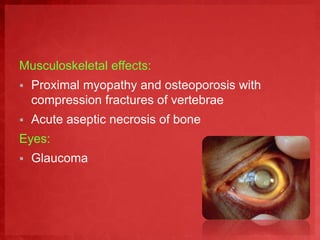
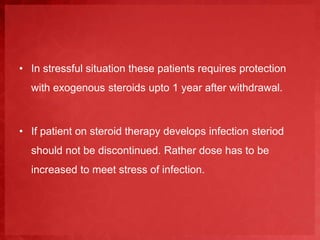
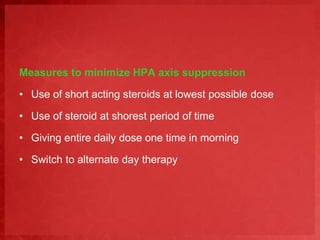
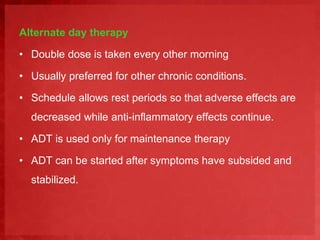
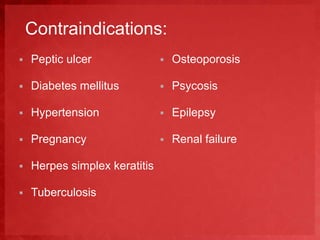
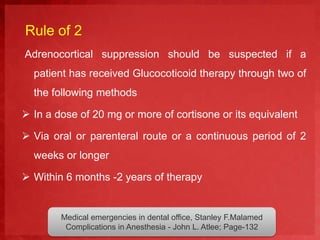
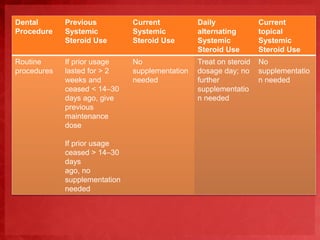
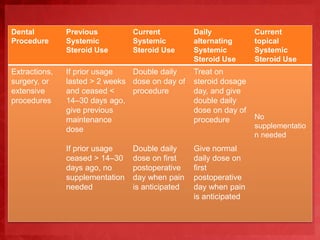
This document discusses corticosteroids, highlighting their importance in regulating metabolism, water balance, and stress responses. It covers their biosynthesis, mechanisms of action, clinical uses in medicine and dentistry, and the potential adverse effects associated with their use. The document also details specific steroid classifications and treatment protocols for various medical conditions, particularly in oral and systemic applications.