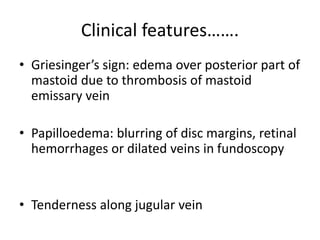
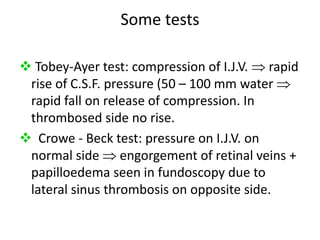
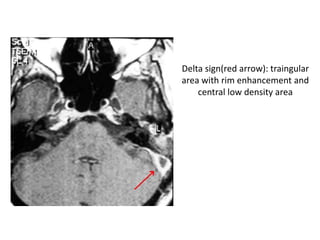
Lateral sinus thrombophlebitis is an inflammation of the inner wall of the lateral venous sinus caused by infection from acute or chronic ear diseases. Bacteria enter the sinus and cause a thrombus formation within the sinus, obstructing drainage. Common symptoms include fever, headache, and papilledema. Diagnosis involves blood tests and imaging like CT or MRI. Treatment requires antibiotics, surgery to drain abscesses and remove clots, and sometimes anticoagulants or jugular vein ligation. Complications can include sepsis, meningitis, abscesses if not treated promptly.