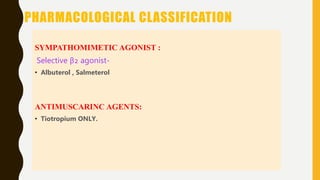
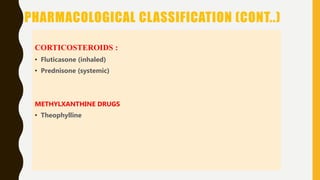
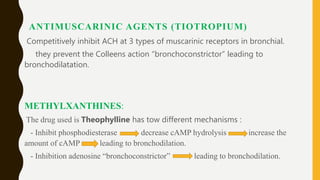
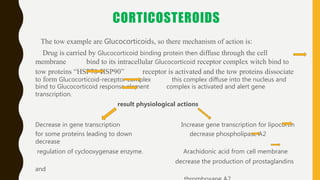
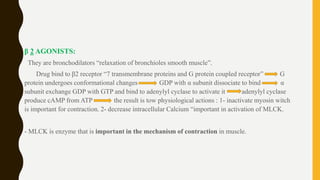
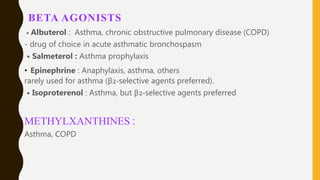
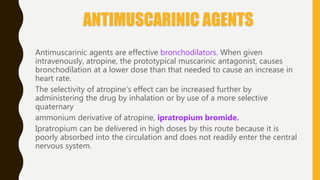
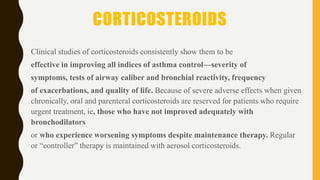
The document discusses chronic obstructive pulmonary disease (COPD) and asthma, highlighting their differences in causes, symptoms, and patient demographics. It also details various pharmacological treatments for both conditions, including sympathomimetic agents, methylxanthines, antimuscarinic agents, and corticosteroids, along with their mechanisms of action and potential side effects. Additionally, it emphasizes the therapeutic uses of these drugs in managing asthma and COPD, and the need for cautious use due to possible adverse effects.