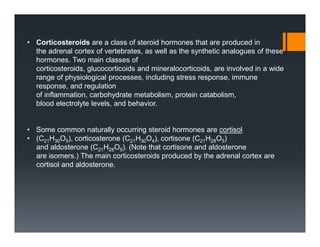
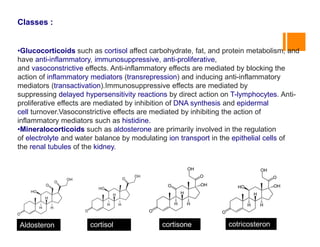
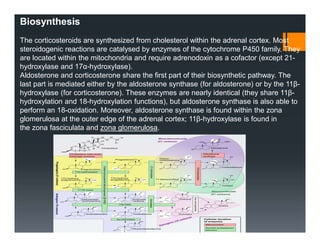
Corticosteroids are a class of steroid hormones that are produced in the adrenal cortex or synthesized. They are involved in processes like stress response and inflammation regulation. The two main classes are glucocorticoids like cortisol and mineralocorticoids like aldosterone. Corticosteroids have anti-inflammatory, immunosuppressive and other effects. They act by binding to glucocorticoid or mineralocorticoid receptors. While corticosteroids can provide benefits for conditions like inflammation, their use also has numerous potential adverse side effects affecting multiple body systems if used long-term or in high doses.