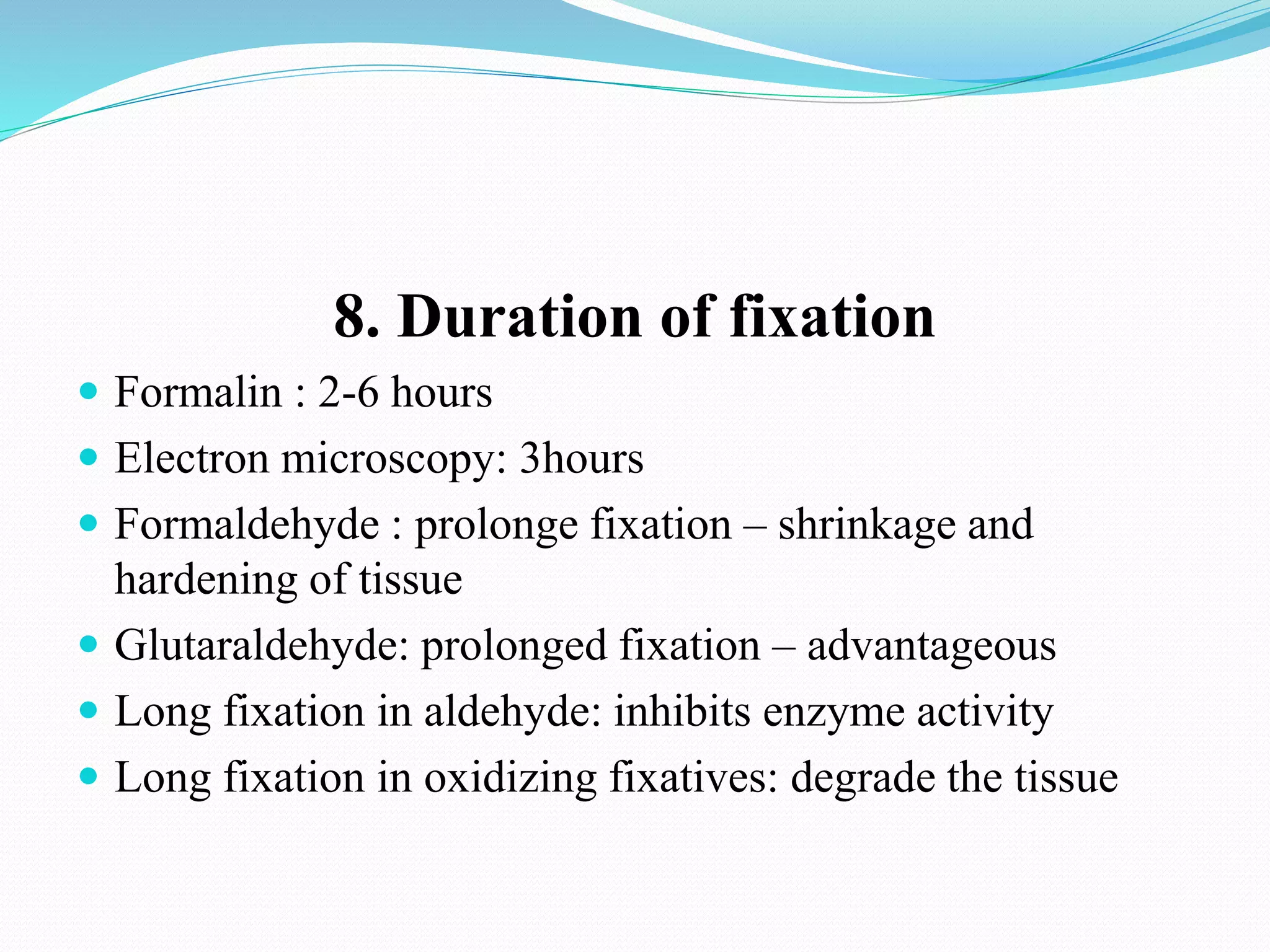
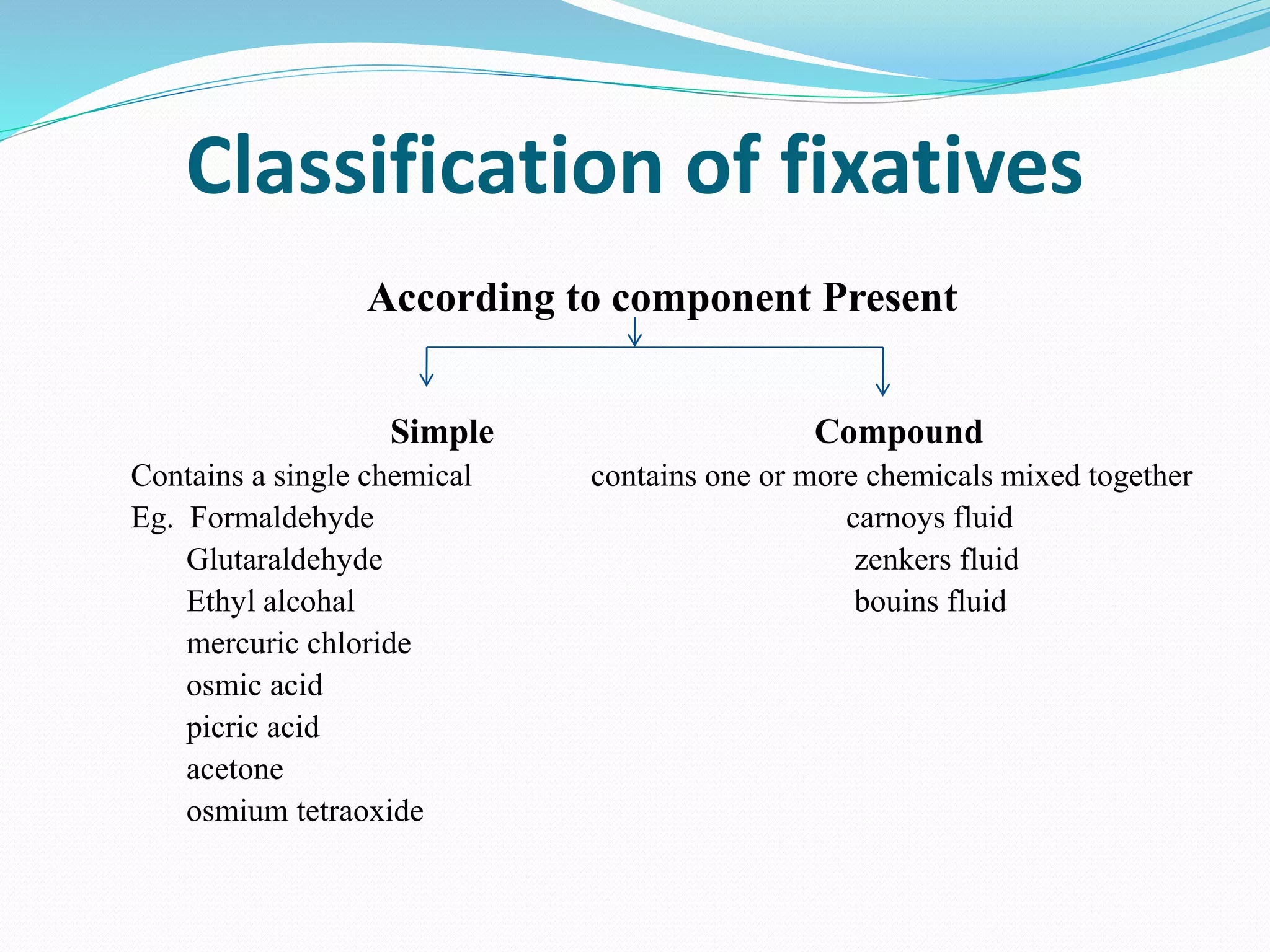
This document discusses histology and histopathology techniques. It defines histology as the study of normal tissue structure and histopathology as the study of diseased tissue structure. It describes various histopathological techniques including tissue fixation, processing, staining and microscopic examination. Several commonly used fixatives are described along with their mechanisms and appropriate tissue and time requirements. Decalcification techniques are also summarized.