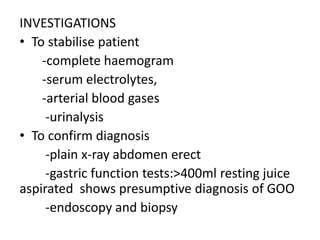
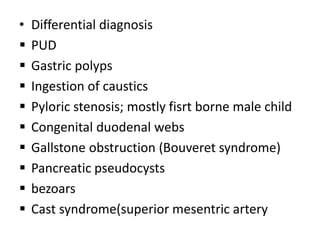
This document describes gastric outlet obstruction (GOO), including its causes, symptoms, examinations, investigations, differential diagnosis, and treatment options. GOO is caused by any mechanical impediment to gastric emptying. Common symptoms include abdominal pain, nausea, vomiting of undigested food, early satiety, and weight loss. Investigations may include blood tests, imaging like x-rays and endoscopy, and gastric function tests. Treatment depends on the underlying cause but may involve resuscitation, antisecretory drugs, endoscopic procedures, or surgery like vagotomy with pyloroplasty or gastric resection. Post-operative complications can include bleeding, strictures, dumping syndrome, and duodenal blowout.