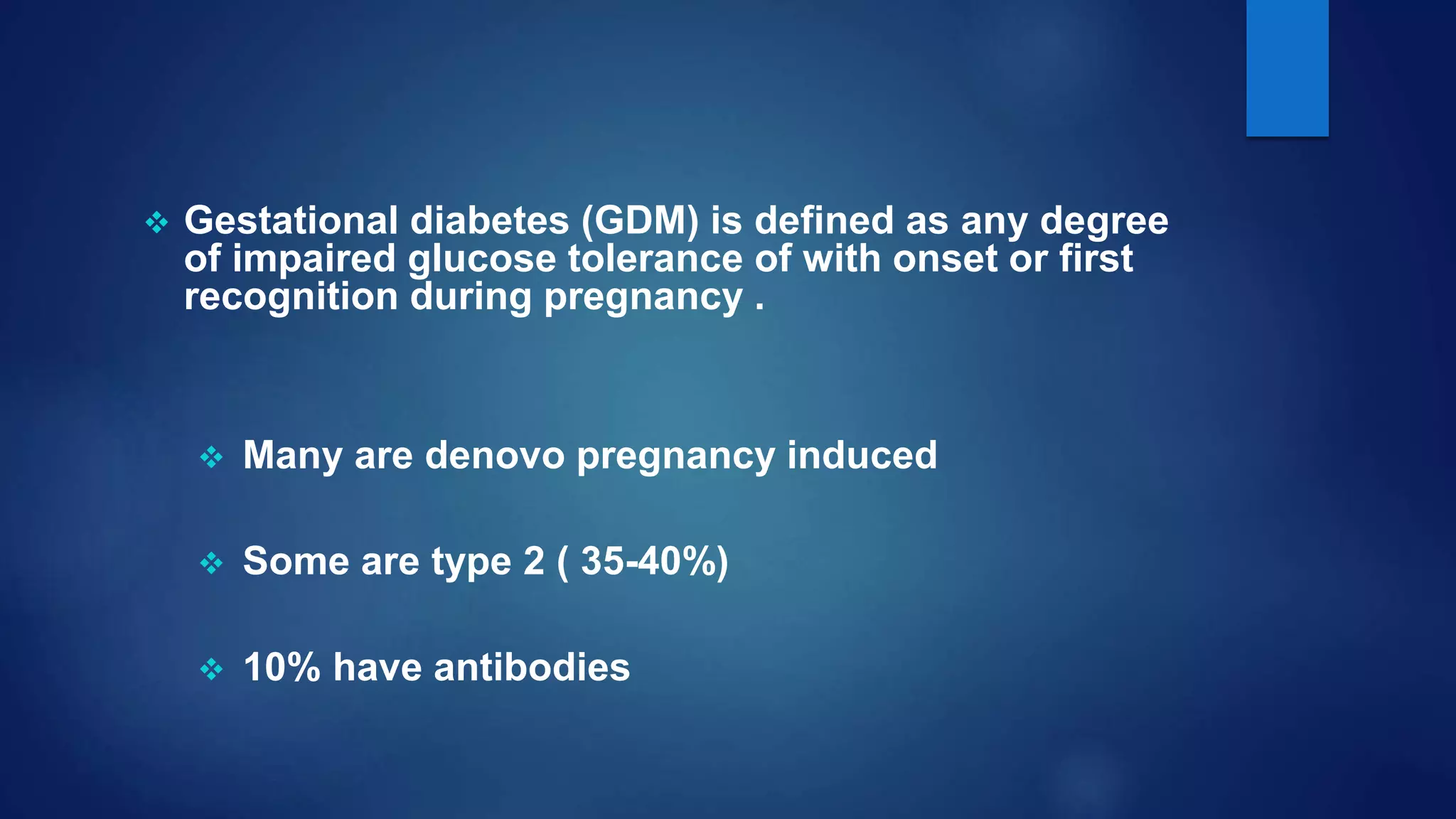
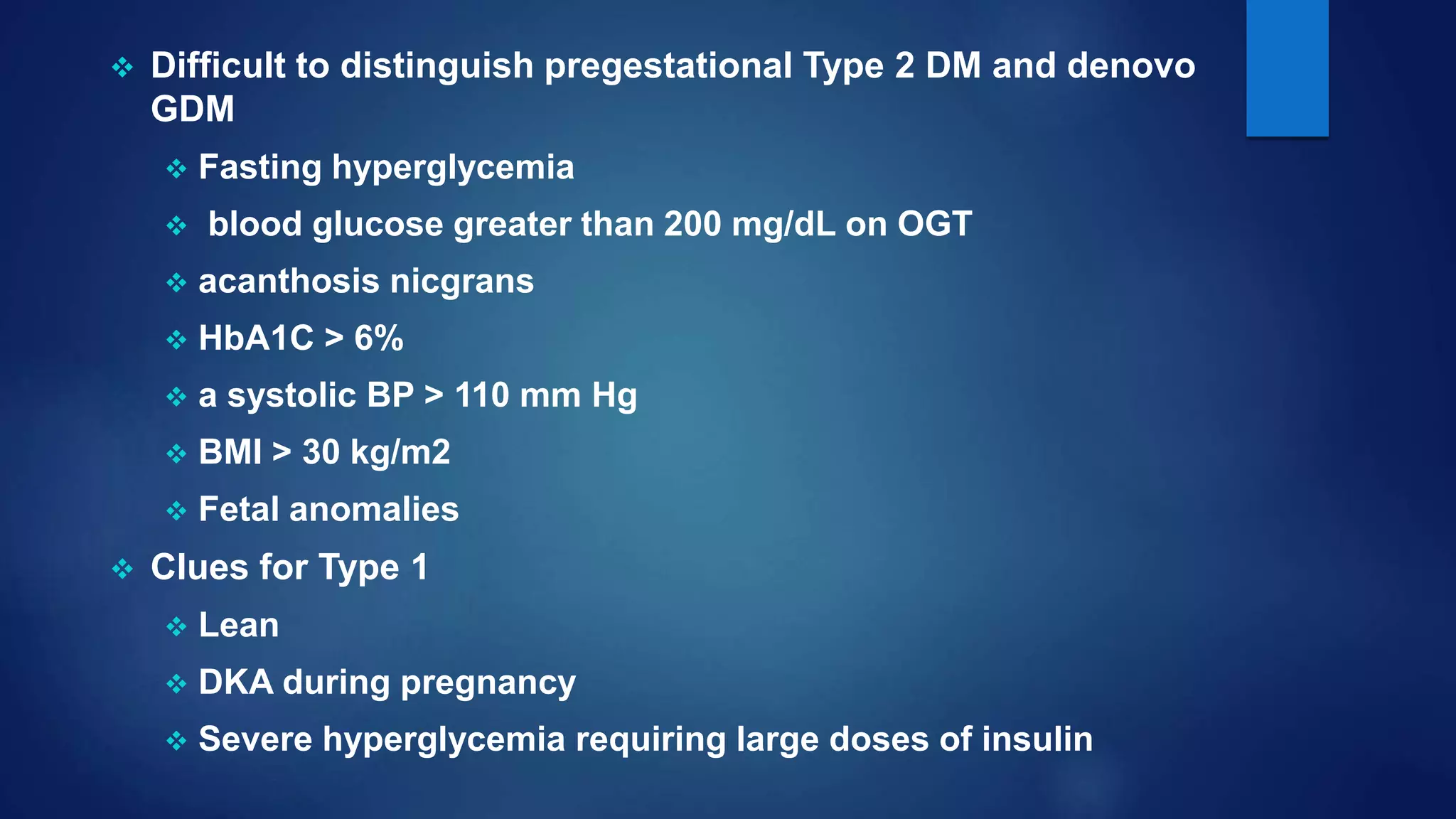
Gestational diabetes (GDM) is glucose intolerance that begins or is first recognized during pregnancy. It can be caused by either pre-existing type 2 diabetes or a new onset of diabetes during pregnancy. The document discusses screening, diagnosis and management of both pre-existing diabetes and GDM during pregnancy. It aims to provide optimal glucose control to support fetal growth while avoiding risks of hyper- and hypoglycemia. Treatment involves medical nutrition therapy, glucose monitoring and may require insulin therapy in some cases. Close monitoring is needed throughout pregnancy and postpartum to support maternal and fetal health.



![RISK FACTORS
History of macrosomia:birth weght>4 Kg,h/o GDM previous
pregnancy
Race
Polycystic ovarian syndrome
Essential hypertension or pregnancy-related hypertension
history of spontaneous abortions and unexplained stillbirths
strong family history of diabetes (especially in first-degree
relatives)
obesity ( [BMI] > 30)
age older than 25 years
persistent glucosuria](https://image.slidesharecdn.com/gestationaldiabetesmellitus-190918054714/75/Gestational-diabetes-mellitus-9-2048.jpg)