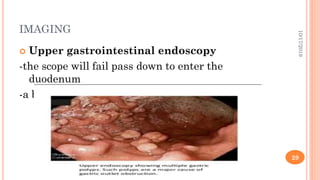
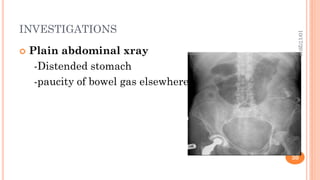
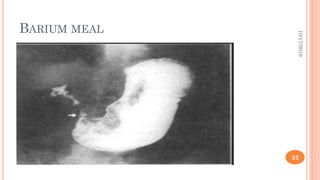
This document provides information on gastric outlet obstruction (GOO), including its definition, causes, pathophysiology, clinical presentation, investigations, and management. It presents the case of a 59-year-old male patient who presented with generalized weakness, postprandial vomiting, and weight loss. Endoscopic biopsy revealed gastric carcinoma known as linitis plastica, resulting in a diagnosis of GOO secondary to gastric malignancy. The document discusses benign and malignant causes of GOO, and the metabolic effects, clinical features, and approach to investigating and initially managing a patient with GOO.